Clock Drawing Test (CDT)
Purpose
The CDT is used to quickly assess visuospatial and praxis abilities, and may determine the presence of both attention and executive dysfunctions (Adunsky, Fleissig, Levenkrohn, Arad, & Nov, 2002; Suhr, Grace, Allen, Nadler, & McKenna, 1998; McDowell, & Newell, 1996).
The CDT may be used in addition to other quick screening tests such as the Mini-Mental State Examination (MMSE), and the Functional Independence Measure (FIM).
In-Depth Review
Purpose of the measure
The CDT is used to quickly assess visuospatial and praxis abilities, and may determine the presence of both attention and executive dysfunctions (Adunsky, Fleissig, Levenkrohn, Arad, & Nov, 2002; Suhr, Grace, Allen, Nadler, & McKenna, 1998; McDowell & Newell, 1996).
The CDT may be used in addition to other quick screening
tests such as the Mini-Mental State Examination (MMSE), and the Functional Independence Measure (FIM).
Available versions
The CDT is a simple task completion test in its most basic form. There are several variations to the CDT:
Verbal command:
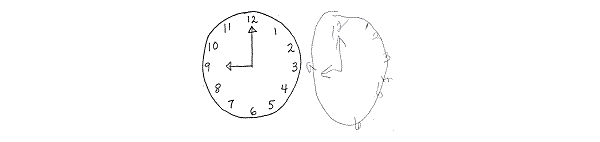
- Free drawn clock:
The individual is given a blank sheet of paper and asked first to draw the face of a clock, place the numbers on the clock, and then draw the hands to indicate a given time. To successfully complete this task, the patient must first draw the contour of the clock, then place the numbers 1 through 12 inside, and finally indicate the correct time by drawing in the hands of the clock. - Pre-drawn clock:
Alternatively, some clinicians prefer to provide the individual with a pre-drawn circle and the patient is only required to place the numbers and the hands on the face of the clock. They argue that the patient’s ability to fill in the numbers may be adversely affected if the contour is poorly drawn. In this task, if an individual draws a completely normal clock, it is a fast indication that a number of functions are intact. However, a markedly abnormal clock is an important indication that the individual may have a cognitive deficit, warranting further investigation.
Regardless of which type is used (free drawn or pre-drawn), the verbal command CDT can simultaneously assess a patient’s language function (verbal comprehension); memory function (recall of a visual engram, short-term storage, and recall of time setting instructions); and executive function. The verbal command variation of the CDT is highly sensitive for temporal lobe dysfunction (due to its heavy involvement in both memory and language processes) and frontal lobe dysfunction (due to its mediation of executive planning
) (Shah, 2002).
Copy command:
The individual is given a fully drawn clock with a certain time pre-marked and is asked to replicate the drawing as closely as possible. The successful completion of the copy command requires less use of language and memory functions but requires greater reliance on visuospatial and perceptual processes.
Clock reading test:
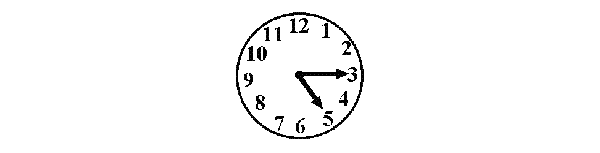
A modified version of the copy command CDT simply asks the patient to read aloud the indicated time on a clock drawn by the examiner. The copy command clock-drawing and clock reading tests are good for assessing parietal lobe lesions such as those that may result in hemineglect. It is important to do both the verbal command and the copy command tests for every patient as a patient with a temporal lobe lesion may copy a pre-drawn clock adequately, whereas their clock drawn to verbal command may show poor number spacing and incorrect time setting. Conversely, a patient with a parietal lobe lesion may draw an adequate clock to verbal command, while their clock drawing with the copy command may show obvious signs of neglect.
Time-Setting Instructions:
The most common setting chosen by clinicians is “3 O’clock” (Freedman, Leach, Kaplan, Winocur, Shulman, & Delis, 1994). Although this setting adequately assesses comprehension and motor execution, it does not indicate the presence of any left neglect the patient may have because it does not require the left half of the clock to be used at all. The time setting “10 after 11” is an ideal setting (Kaplan, 1988). It forces the patient to attend to the whole clock and requires the recoding of the command “10” to the number “2” on the clock. It also has the added advantage of uncovering any stimulus-bound errors that the patient may make. For example, the presence of the number “10” on the clock may trap some patients and prevent the recoding of the command “10” into the number “2.” Instead of drawing the minute hand towards the number “2” on the clock to indicate “10 after,” patients prone to stimulus-bound errors will fixate and draw the minute hand toward the number “10” on the clock.
Features of the measure
Scoring:
There are a number of different ways to score the CDT. In general, the scores are used to evaluate any errors or distortions such as neglecting to include numbers, putting numbers in the wrong place, or having incorrect spacing (McDowell & Newell, 1996). Scoring systems may be simple or complex, quantitative or qualitative in nature. As a quick preliminary screening
tool to simply detect the presence or absence of cognitive impairment, you may wish to use a simple quantitative method (Lorentz et al., 2002). However, if a more complex assessment is required, a qualitative scoring system would be more telling.
Different scoring methods have been found to be better suited for different subject groups (Richardson & Glass, 2002; Heinrik, Solomesh, & Berkman, 2004). In patients with stroke
A psychometric study in patients with stroke
Subscales:
None typically reported.
Equipment:
Only a paper and pencil is required. Depending on the method chosen, you may need to prepare a circle (about 10 cm in diameter) on the paper for the patient.
Training:
The CDT can be administered by individuals with little or no training in cognitive assessment. Scanlan, Brush, Quijano, & Borson (2002) found that a simple binary rating of clock drawings (normal or abnormal) by untrained raters was surprisingly effective in classifying subjects as having dementia or not. In this study, a common mistake of untrained scorers was failure to recognize incorrect spacing of numbers on the clock face as abnormal. By directing at this type of error, concordance between untrained and expert raters should improve.
Time:
All variations of the CDT should take approximately 1-2 minutes to complete (Ruchinskas & Curyto, 2003).
Alternative forms of the CDT
The Clock Drawing Test-Modified and Integrated Approach (CDT-MIA) is a 4-step, 20-item instrument, with a maximum score of 33. The CDT-MIA emphasizes differential scoring of contour, numbers, hands, and center. It integrates 3 existing CDT’s:
- Freedman et al’s free-drawn clock (1994) on some item definitions
- Scoring techniques adapted from Paganini-Hill, Clark, Henderson, & Birge (2001)
- Some items borrowed from Royall, Cordes, & Polk (1998) executive CLOX
The CDT-MIA was found to be reliable and valid in individuals with dementia, however this measure has not been validated in the stroke
Client suitability
Can be used as a screening instrument with:
Virtually any patient population (Wagner, Nayak, & Fink, 1995). The test appears to be differentially sensitive to some types of disease processes. Particularly, it has proven to be clinically useful in differentiating among normal elderly, patients with neurodegenerative or vascular diseases, and those with psychiatric disorders, such as depression
and schizophrenia (Dastoor, Schwartz, & Kurzman, 1991; Heinik, Vainer-Benaiah, Lahav, & Drummer, 1997; Lee & Lawlor, 1995; Shulman, Gold, & Cohen, 1993; Spreen & Strauss, 1991; Tracy, De Leon, Doonan, Musciente, Ballas, & Josiassen, 1996; Wagner et al., 1995; Wolf-Klein, Silverstone, Levy, & Brod, 1989).
Can be used with:
- Patients with stroke
Also called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain.. Because the CDT requires a nonverbal response, it may be administered to those with speech difficulties but who have sufficient comprehension to understand the requirement of the task.
Should not be used in:
- Patients who cannot understand spoken or written instructions
- Patients who cannot write
As with many other neuropsychological screening
measures, the CDT is affected by age, education, conditions such as visual neglect and hemiparesis, and other factors such as the presence of depression
(Ruchinskas & Curyto, 2003; Lorentz, Scanlan, & Borson, 2002). The degree to which these factors affect ones score depends much on the scoring method applied (McDowell & Newell, 1996). Moreover, the CDT focuses on right hemisphere function, so it is important to use this test in conjunction with other neuropsychological tests (McDowell & Newell, 1996).
In what languages is the measure available?
The CDT can be conducted in any language. Borson et al. (1999) found that language spoken did not have any direct effect on CDT test performance.
Summary
| What does the tool measure? | Visuospatial and praxis abilities, and may determine the presence of both attention and executive dysfunctions. |
| What types of clients can the tool be used for? | Virtually any patient population. It has proven to be clinically useful in differentiating among normal elderly, patients with neurodegenerative or vascular diseases, and those with psychiatric disorders, such as depression and schizophrenia. |
| Is this a screening or assessment tool? |
Screening |
| Time to administer | All variations of the CDT should take approximately 1-2 minutes to complete. |
| Versions |
|
| Languages | The CDT can be conducted in any language. |
| Measurement Properties | |
| Reliability |
Test-retest: Out of four studies examining test-retest reliability , three reported excellent test-retest and 1 found adequate test-retest. Inter-rater: Out of seven studies examining inter-rater reliability , six reported excellent inter-rater and one reported adequate (for examiner clocks) to excellent (for free-drawn and pre-drawn clocks inter-rater. |
| Validity |
Criterion: Predicted lower functional ability and increased need for supervision on hospital discharge; poor physical ability and longer length of stay in geriatric rehabilitation; activities of daily living at maximal recovery. Construct: The CDT correlated adequately with the Mini-Mental State Examination and the Functional Independence Measure. Known groups: Significant differences between Alzheimer’s patients and controls detected by CDT. |
| Does the tool detect change in patients? | Not applicable |
| Acceptability | The CDT is short and simple. It is a nonverbal task and may be less threatening to patients than responding to a series of questions. |
| Feasibility | The CDT is inexpensive and highly portable. It can be administered in situations in which longer tests would be impossible or inconvenient. Even the most complex administration and scoring system requires approximately 2 minutes. It can be administered by individuals with minimal training in cognitive assessment. |
| How to obtain the tool? | A pre-drawn circle can be downloaded by clicking on this link: pre-drawn circle |
Psychometric Properties
Overview
Until recently, data on the psychometric properties of the CDT were limited. While there are many possible ways to administer and score the CDT, the psychometric properties of all the various systems seem consistent and all forms correlate strongly with other cognitive measures (Scanlan et al., 2002; Ruchinskas & Curyto, 2003; McDowell & Newell, 1996). Further, scoring of the CDT has been found to be both accurate and consistent in patients with stroke
For the purposes of this review, we conducted a literature search to identify all relevant publications on the psychometric properties of the more commonly applied scoring methods of the CDT. We then selected to review articles from high impact journals, and from a variety of authors.
Reliability
Test-retest:
Using Spearman rank order correlations of the CDT has been reported by several investigators using a variety of scoring systems:
- Manos and Wu (1994) reported an “excellent” 2-day test-retest reliability
A way of estimating the reliability of a scale in which individuals are administered the same scale on two different occasions and then the two scores are assessed for consistency. This method of evaluating reliability is appropriate only if the phenomenon that the scale measures is known to be stable over the interval between assessments. If the phenomenon being measured fluctuates substantially over time, then the test-retest paradigm may significantly underestimate reliability. In using test-retest reliability, the investigator needs to take into account the possibility of practice effects, which can artificially inflate the estimate of reliability (National Multiple Sclerosis Society).
of 0.87 for medical patients and 0.94 for surgical patients. - Tuokko et al. (1992) reported an “adequate” test-retest reliability
A way of estimating the reliability of a scale in which individuals are administered the same scale on two different occasions and then the two scores are assessed for consistency. This method of evaluating reliability is appropriate only if the phenomenon that the scale measures is known to be stable over the interval between assessments. If the phenomenon being measured fluctuates substantially over time, then the test-retest paradigm may significantly underestimate reliability. In using test-retest reliability, the investigator needs to take into account the possibility of practice effects, which can artificially inflate the estimate of reliability (National Multiple Sclerosis Society).
of 0.70 at 4 days. - Mendez et al. (1992) reported and “excellent” coefficients of 0.78 and 0.76 at 3 and 6 months, respectively.
- Freedman et al. (1994) reported test-retest reliability
A way of estimating the reliability of a scale in which individuals are administered the same scale on two different occasions and then the two scores are assessed for consistency. This method of evaluating reliability is appropriate only if the phenomenon that the scale measures is known to be stable over the interval between assessments. If the phenomenon being measured fluctuates substantially over time, then the test-retest paradigm may significantly underestimate reliability. In using test-retest reliability, the investigator needs to take into account the possibility of practice effects, which can artificially inflate the estimate of reliability (National Multiple Sclerosis Society).
as “very low”. However, when the “10 after 11” time setting was used with the examiner clock, which is known to be a more sensitive setting for detecting cognitive dysfunction, test-retest reliabilityA way of estimating the reliability of a scale in which individuals are administered the same scale on two different occasions and then the two scores are assessed for consistency. This method of evaluating reliability is appropriate only if the phenomenon that the scale measures is known to be stable over the interval between assessments. If the phenomenon being measured fluctuates substantially over time, then the test-retest paradigm may significantly underestimate reliability. In using test-retest reliability, the investigator needs to take into account the possibility of practice effects, which can artificially inflate the estimate of reliability (National Multiple Sclerosis Society).
was found to be “excellent” (0.94).
Inter-rater:
Inter-rater reliability
of the CDT, as indicated by Spearman rank order correlations (not the preferred method of analyses for assessing inter-rater reliability
but one used in earlier measurement research), has also been reported by several investigators:
- Sunderland et al. (1989) found “excellent” coefficients ranging from 0.86 to 0.97 and found no difference between clinician and non-clinician raters (0.84 and 0.86, respectively).
- Rouleau et al. (1992) found “excellent” inter-rater reliability
A method of measuring reliability . Inter-rater reliability determines the extent to which two or more raters obtain the same result when using the same instrument to measure a concept.
, with coefficients ranging from 0.92 to 0.97. - Mendez et al. (1992) reported “excellent” inter-rater reliability
A method of measuring reliability . Inter-rater reliability determines the extent to which two or more raters obtain the same result when using the same instrument to measure a concept.
of 0.94. - Tuokko et al. (1992) reported high coefficients ranging from 0.94 to 0.97 across three annual assessments.
- The modified Shulman scale (Shulman, Gold, Cohen, & Zucchero, 1993) also has “excellent” inter-rater reliability
A method of measuring reliability . Inter-rater reliability determines the extent to which two or more raters obtain the same result when using the same instrument to measure a concept.
(0.94 at baseline, 0.97 at 6 months, and 0.97 at 12 months). - Manos and Wu (1994) obtained “excellent” inter-rater reliability
A method of measuring reliability . Inter-rater reliability determines the extent to which two or more raters obtain the same result when using the same instrument to measure a concept.
coefficients ranging from 0.88 to 0.96. - Freedman et al. (1994) reported coefficients ranging from 0.79 to 0.99 on the free-drawn clocks, 0.84 to 0.85 using the pre-drawn contours, and 0.63 to 0.74 for the examiner clocks, demonstrating “excellent” inter-rater reliability
A method of measuring reliability . Inter-rater reliability determines the extent to which two or more raters obtain the same result when using the same instrument to measure a concept.
.
South et al. (2001) compared the psychometrics of 3 different scoring methods of the CDT (Libon revised system; Rouleau rating scale; and Freedman scoring system) in a sample of 20 patients with stroke
were measured using the intraclass correlation coefficient (ICC)
. Raters used similar scoring criteria throughout, demonstrating “excellent” intra-rater reliability
. South et al. (2001) concluded that while the Libon scoring system demonstrated a range of reliabilities across different domains, the Rouleau and Freedman systems were in the excellent range.
Validity
In a review, Shulman (2000) reported that most studies achieved sensitivities and specificities of approximately 85% and concluded that the CDT, in conjunction with other widely used tests such as the Mini-Mental State Examination (MMSE), could provide a significant advance in the early detection of dementia. In contrast, Powlishta et al. (2002) concluded from their study that the CDT did not appear to be a useful screening
tool for detecting very mild dementia. Other authors have concluded that the CDT should not be used alone as a dementia screening
test because of its overall inadequate performance (Borson & Brush, 2002; Storey et al., 2001). However, most of the previous studies were based on relatively small sample sizes or were undertaken in a clinical setting, and their results may not be applicable to a larger community population.
Nishiwaki et al. (2004) studied the validity
of the CDT in comparison to the MMSE in a large general elderly population (aged 75 years or older). The specificity
of the CDT for detecting moderate-to-severe cognitive impairment (MMSE score = 17) were 77% and 87%, respectively, for nurse
administration and 40% and 91%, respectively, for postal administration. The authors conclude that the CDT may have value as a brief face-to-face screening
tool for moderate/severe cognitive impairment in an older community population but is relatively poor at detecting milder cognitive impairment.
Few studies have examined the validity
of the CDT specifically in patients with stroke
coefficients (Pearson correlation
) between the three cognitive tests resulted in r-values ranging from 0.51 to 0.59. Adunsky et al. (2002) concluded that they share a reasonable degree of resemblance to each other, accounting for “adequate” concurrent validity
of these tests.
Bailey, Riddoch, and Crome (2000) evaluated a test battery for hemineglect in elderly patients with stroke
in the assessment of representational neglect. Further, consistent with previous findings (Ishiai et al., 1993; Kaplan et al., 1991), the utility of the CDT as a screening
measure for neglect was not supported from these results. Reasons include the subjectivity in scoring, and questionable validity
in that the task may also reflect cognitive impairment (Freidman, 1991), constructional apraxia, or impaired planning
ability (Kinsella, Packer, Ng, Olver, & Stark, 1995).
Responsiveness
Not applicable.
References
- Adunsky, A., Fleissig, Y., Levenkrohn, S., Arad, M., Nov, S.(2002). Clock drawing task, mini-mental state examination and cognitive-functional independence measure: relation to functional outcome of stroke patients. Arch Gerontol Geriatr, 35(2), 153-60.
- Bailey, M. J., Riddoch, J., Crome, P. (2002). Evaluation ofa test battery for hemineglect in elderly stroke patients for use by therapists in clinical practice. Neurorehabilitation, 14(3), 139-150.
- Borson, S., Brush, M., Gil, E., Scanlan, J., Vitaliano, P.,Chen, J., Cahsman, J., Sta Maria, M. M., Barnhart, R., Roques, J. (1999). The Clock Drawing Test: Utility for dementia detection in multiethnic elders. J Gerontol A Biol Sci Med Sci, 54, M534-40.
- Dastoor, D. P., Schwartz, G., Kurzman, D. (1991).Clock-drawing: An assessment technique in dementia. Journal of Clinical and Experimental Gerontology, 13, 69-85.
- Freedman, M., Leach, L., Kaplan, E., Winocur, G., Shulman,K. I., Delis, D. C. (1994). Clock Drawing: A Neuropsychological Analysis (pp. 5). New York: Oxford University Press.
- Friedman, P. J. (1991). Clock drawing in acute stroke.Age and Ageing, 20(2), 140-145.
- Heinik, J., Vainer-Benaiah, Z., Lahav, D., Drummer, D.(1997). Clock drawing test in elderly schizophrenia patients. International Journal of Geriatric Psychiatry, 12, 653-655.
- Heinik, J., Solomesh, I., Berkman, P. (2004). Correlationbetween the CAMCOG, the MMSE and three clock drawing tests in a specialized outpatient psychogeriatric service. Arch Gerontol Geriatr, 38, 77-84.
- Heinik, J., Solomesh, I., Lin, R., Raikher, B., Goldray, D.,Merdler, C., Kemelman, P. (2004). Clock drawing test-modified and integrated approach (CDT-MIA): Description and preliminary examination of its validity and reliability in dementia patients referred to a specialized psychogeriatric setting. J Geriatr Psychiatry Neurol, 17, 73-80.
- Ishiai, S., Sugishita, M., Ichikawa, T., Gono, S., Watabiki,S. (1993). Clock drawing test and unilateral spatial neglect. Neurology, 43, 106-110.
- Kaplan, E. (1988). A process approach to neuropsychologicalassessment. In: T Bull & BK Bryant (Eds.), Clinical neuropsychology and brain function: Research, measurement, and practice (pp. 129-167). Washington DC: American Psychological Association.
- Kaplan, R.F., Verfaillie, M., Meadows, M., Caplan, L.R.,Pessin, M. S., DeWitt L. (1991). Changing attentional demands in left hemispatial neglect. Archives of Neurology, 48, 1263-1267.
- Kinsella, G., Packer, S., Ng, K., Olver, J., Stark, R.(1995). Continuing issues in the assessment of neglect. Neuropsychological Rehabilitation, 5, 239-258.
- Lee, H., Lawlor, B. A. (1995). State-dependent nature of theClock Drawing Task in geriatric depression. Journal of the American Geriatrics Society, 43, 796-798.
- Lorentz, W. J., Scanlan, J. M., Borson, S. (2002). Briefscreening tests for dementia. Can J Psychiatry, 47, 723-733.
- Manos, P. J., Wu, R. (1994). The Ten Point Clock Test: Aquick screen and grading system for cognitive impairment in medical and surgical patients. International Journal of Psychiatry in Medicine, 24, 229-244.
- McDowell, I., Newell, C. (1996). Measuring Health. A Guideto Rating Scales and Questionnaires. 2nd ed. NewYork: Oxford University Press.
- Mendez, M. F., Ala, T., Underwood, K. L. (1992). Developmentof scoring criteria for the clock drawing task in Alzheimers disease. Journal of the American Geriatrics Society, 40, 1095-1099.
- Nishiwaki, Y., Breeze, E., Smeeth, L., Bulpitt, C. J.,Peters, R., Fletcher, A. E. (2004). Validity of the Clock-Drawing Test as a Screening Tool for Cognitive Impairment in the Elderly. American Journal of Epidemiology, 160(8), 797-807.
- Paganini-Hill, A., Clark, L. J., Henderson, V. W., Birge, S.J. (2001). Clock drawing: Analysis in a retirement community. J Am Geriatr Soc, 49, 941-947.
- Powlishta, K. K., von Dras, D. D., Stanford, A., Carr D. B.,Tsering, C., Miller, J. P., Morris, J. C. (2002). The Clock Drawing Test is a poor screen for very mild dementia. Neurology, 59, 898-903.
- Richardson, H. E., Glass, J.N. (2002). A comparison ofscoring protocols on the clock drawing test in relation to ease of use, diagnostic group and correlations with mini-mental state examination. Journal of the American Geriatrics Society, 50, 169-173.
- Rouleau, I., Salmon, D. P., Butters, N., Kennedy, C.,McGuire, K. (1992). Quantitative and qualitative analyses of clock drawings in Alzheimers and Huntington’s. Brain and Cognition, 18, 70-87.
- Royall, D. R., Cordes, J. A., Polk, M. (1998). CLOX: anexecutive clock drawing task. J Neurol Neurosurg Psychiatry, 64, 588-594.
- Ruchinskas, R. A., Curyto, K. J. (2003). Cognitive screeningin geriatric rehabilitation. Rehabil Psychol, 48, 14-22.
- Scanlan, J. M., Brush, M., Quijano, C., Borson, S. (2002).Comparing clock tests for dementia screening: naïve judgments vs formal systems – what is optimal? International Journal of Geriatric Psychiatry, 17(1), 14-21.
- Shah, J. (2001). Only time will tell: Clock drawing as anearly indicator of neurological dysfunction. P&S Medical Review, 7(2), 30-34.
- Shulman, K. I., Gold, D. P., Cohen, C. A., Zucchero, C. A.(1993). Clock-drawing and dementia in the community: A longitudinal study. International Journal of Geriatric Psychiatry, 8(6), 487-496.
- Shulman, K. I. (2000). Clock-drawing: Is it the idealcognitive screening test? International Journal of Geriatric Psychiatry, 15, 548-561.
- Shulman, K., Shedletsky, R., Silver, I. (1986). Thechallenge of time: Clock-drawing and cognitive function in the elderly. International Journal of Geriatric Psychiatry, 1, 135-140.
- South, M. B., Greve, K. W., Bianchini, K. J., Adams, D.(2001). Inter-rater reliability of Three Clock Drawing Test scoring systems. Applied Neuropsychology, 8(3), 174-179.
- Spreen, O., Strauss, E. A. (1991). Compendium ofneuropsychological tests: Administration, norms, and commentary. New York: Oxford University Press.
- Storey, J. E., Rowland, J. T., Basic, D., Conforti, D. A.(2001). A comparison of five clock scoring methods using ROC (receiver operating characteristic) curve analysis. Int J Geriatr Psychiatr, 16, 394-9.
- Sunderland, T., Hill, J. L., Mellow, A. M., Lowlor, B. A.,Grundersheimer, J., Newhouse, P. A., Grafman, J. H. (1989). Clock drawing in Alzheimer’s disease: a novel measure of dementia severity. J Am Geriatr Soc, 37(8), 725-729.
- Suhr, J., Grace, J., Allen, J., Nadler, J., McKenna, M.(1998). Quantitative and Qualitative Performance of Stroke Versus Normal Elderly on Six Clock Drawing Systems. Archives of Clinical Neuropsychology, 13(6), 495-502.
- Tracy, J. I., De Leon, J., Doonan, R., Musciente, J.,Ballas, T., Josiassen, R. C. (1996). Clock drawing in schizophrenia. Psychological Reports, 79, 923-928.
- Tuokko, H., Hadjistavropoulos, T., Miller, J. A., Beattie,B. L. (1992). The Clock Test, a sensitive measure to differentiate normal elderly from those with Alzheimer disease. Journal of the American Geriatrics Society, 40, 579-584.
- Wagner, M. T., Nayak, M., Fink, C. (1995). Bedside screeningof neurocognitive function. In: L. A. Cushman & M. J. Scherer (Eds.), Psychological assessment in medical rehabilitation: Measurement and instrumentation in psychology (pp. 145-198). Washington, DC: American Psychological Association.
- Watson, Y. I., Arfken, C. L., Birge, S. J. (1993). Clockcompletion : An objective screening test for dimentia. J Am Geriar Soc, 41(11), 1235-40.
- Wolf-Klein, G. P., Silverstone, F. A., Levy, A. P., Brod, M.S. (1989). Screening for Alzheimer’s disease by clock drawing.Journal of the American Geriatrics Society, 37, 730-734.
See the measure
Click here to find a pre-drawn circle that can be used when administering the CDT.