Unilateral Spatial Neglect
Introduction
Unilateral spatial neglect (USN) is one of the disabling features of a stroke, and is defined as a failure to attend to the side opposite a brain lesion. Clinically, the presence of severe USN is apparent when a patient often collides into his/her surroundings, ignores food on one side of the plate, and attends to only one side of his/her body. Many terms are used interchangeably in the literature to describe USN, such as unilateral neglect, hemi-inattention, visual neglect and hemi spatial neglect. It is estimated that as many as 30% of patients experience USN following a stroke.
A client with USN is unable to attend to either one side of his/her body (personal neglect), the space within reaching distance (near extrapersonal neglect), the space beyond reaching distance (far extrapersonal neglect), or to a combination of these three spaces in the environment. USN continues to be commonly associated with a right stroke, but evidence from the literature suggests that all patients with stroke might benefit from USN screening.
The presence of USN has been strongly associated with an increased risk for injury and with poor functional outcomes. The effects of USN extend beyond the basic skills for self-care (bathing, dressing, walking, etc.) to instrumental activities of daily living (IADL) that are crucial for successful reintegration into community life.
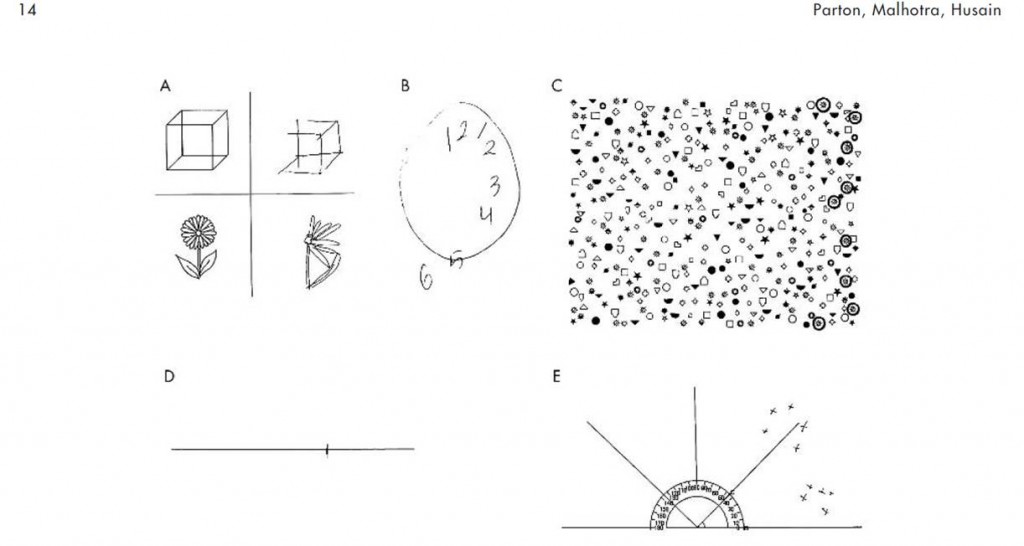
When refering to the figure below “Typically, right hemisphere patients with left neglect omit elements to their left when copying simple objects (A), drawing a clock face (B), and cancelling targets among distractors (C). They also tend to err to the right when asked to bisect a horizontal line (D). When asked to name objects in their surroundings, they will tend to name only those on the right. Crosses in (E) mark the locations of reported objects with respect to the patient.” (page 14 from Parton, A et al. J Neurol Neurosurg Psychiatry 2004; 75:13-21 reproduced with permission from the BMJ Publishing Group).
Patient/Family Information
What is unilateral spatial neglect?
Unilateral spatial neglect (USN) is the inability to pay attention to people and things on the side that is affected by the stroke. For example, someone with left-sided paralysis may also have left-sided USN. This problem is sometimes called unilateral visual neglect.
Picture of the Clock Drawing Test of a normal individual (right) and a patient with left neglect (left)
Patients with severe USN have obvious symptoms in that they may:
- Collide into their surroundings on one side (usually the left) when trying to wheel a wheelchair,
- Ignore food on one side of the plate, usually the left half,
- Ignore one side of their body, usually the left.
For example, you might notice that a person with USN shaves only one half of his face, typically the right, while ignoring the left.
Family members often become frustrated in the early days after the stroke because they do not understand why the patient is not looking at them when they stand on the side affected by the stroke. It is because the person is unaware of that side, not because they are ignoring you.
A patient can also have mild symptoms of USN that are not as obvious. For example, he may be able to notice food on both the left and right side, and may look at you if you are on his affected side, but may have difficulty with more complex daily tasks, such as driving a car or crossing a busy street.
Because USN can result in falls and other problems when doing daily activities, and because it is treatable, it is important that all patients who have had a stroke receive at least a quick assessment to test for USN.
How frequent is USN after a stroke?
About 30% of patients have either hemianopsia (blindness on one side of both eyes) or USN following stroke. USN is found more often in those who have had a stroke in the right side of the brain. However, studies show that all patients with stroke should receive testing for USN. USN can occur in three ways:
- A person may have USN that results in neglect of one side of their body. For example, you may notice a person whose hand is hanging over into the wheelchair spokes but he doesn’t realize it.
- A person may have USN in the space within reaching distance. For example, you may notice that the person does not know where the telephone is, even when it is fairly close by, because it is on the side affected by the stroke.
- A person may have USN in the space beyond reaching distance. This type of USN is often missed while the patient is in the hospital, but it is serious because when walking and driving, the person is missing important visual information from one half of the environment.
Neglect can occur in all of these three ways or in a combination of these.
What are the potential consequences of having USN after a stroke?
Those with USN are more at risk to fall and usually have lower functional ability than those without USN. USN can affect the ability to take care of basic skills such as bathing, dressing, and walking.
Can USN caused by a stroke be treated?
There are four types of treatment for USN:
- Visual Scanning: During this treatment the person with USN is encouraged to explore the neglected visual field (usually the left side) by performing a task on that side. The treatment often includes a visual target that the patient uses as an anchor while scanning.
- Sensory Stimulation: The therapist uses different types of sensory stimulation to encourage the person to pay attention to their neglected side. These include:
- Visual/Verbal/Auditory Cues: The use of a visual cue (i.e. use of red tape or flashing lights), verbal cue (i.e. the voice of the therapist or a family member) or auditory cue (i.e. horn or bell) on the neglected side to improve awareness of that space.
- Limb Activation: When doing this treatment the patient makes movements of the affected arm and hand on the neglected side to encourage scanning of that space (usually the left hand and arm towards the left). The person receiving treatment can do these movements alone or with help from the therapist.
- Caloric Stimulation: This treatment uses either cold or warm water that is put into the patient’s ear (external ear canal) to encourage scanning of the neglected side. Cold water seems to encourage scanning toward the stimulated ear. Warm water encourages scanning of the field opposite to the stimulated ear.
- Eye Patching/Hemiglasses: This treatment uses standard eyeglass frames with half of both lenses blacked out on the same side (usually the right half). This forces the patient to look through the side of the lens that represents the side that he is ignoring (usually the left side).
- Fresnel Prisms: This treatment involves putting prisms over regular eyeglass frames. The prisms cause a shift of the visual field. So, if there is neglect on the right side, these prisms will cause what is seen to the right to be shifted farther to the right in order to encourage visual scanning of the right visual field. When first wearing these glasses, patients initially reach too far for objects on the right side because their vision is further deviated toward the right. After repeated treatments, clients can correct how far they reach and can accurately grasp the object, despite the distorted visual input they receive with their glasses.
- Neck/Hand Vibration or Stimulation: This intervention consists of the use of vibration or stimulation on the neck or hand of the side affected by the stroke to encourage the patient to look to that side.
- Trunk Rotation: This strategy involves twisting the trunk toward the side affected by USN to improve visual scanning of that space.
- Visuo-motor Imagery: Visual imagery involves mental imaging tasks where the patient is required to describe details of a familiar room, environment, or geographic area. Motor imagery consists of the patient imagining a body movement or posture and describing this sequence. This type of imagery treatment may stimulate areas of the brain that can activate those actual movements during daily activities in order to improve neglect symptoms.
- Constraint-Induced Therapy: This treatment involves restraining the arm that is not affected by the stroke (for example with a sling) to encourage use of the arm affected by the stroke. While used primarily to encourage use of the arm, this intervention will also encourage visual scanning of the side being used.
- Optokinetic Stimulation: This is the observation of moving visual targets from left to right. This treatment is used to encourage visual scanning of the side that is neglected. See here for an example.
- video Feedback: This treatment involves filming the patient while he does specific activities. The therapist and patient then watch the video together. The therapist points out to the client how they are neglecting their body or the space on the side of their body. They then discuss strategies to encourage attention to the patient’s body and the space he is neglecting.
- Pharmacological Therapy: This involves the use of specific medications (dopamine-agonist drugs) to improve visual attention skills. A physician must prescribe these medications.
Which treatment for USN works?
The benefits of various interventions to treat USN symptoms have been carefully studied post-stroke. Research studies have reported that the use of visual scanning, limb activation, trunk rotation, as well as cueing (visual, verbal, auditory) during treatment has led to improvements in USN symptoms and in some cases, improvements in performing daily activities. Patients receiving eye patching and prism therapy have also shown some progress in attending to the neglected side, however, these benefits were only temporary, lasting a few hours after treatment. The other treatments described in the section above require further research before their effectiveness can be confirmed.
Who provides the treatment?
Occupational therapists (OT) typically provide therapy for USN at an acute care hospital, rehabilitation centre, or private clinic.
Clinician Information
The effectiveness of the various interventions in the management of unilateral spatial neglect (USN) has been examined with individuals post-stroke. This review presents 16 high quality RCTs, 14 fair quality RCTs, four poor quality RCTs and several non-randomized studies that evaluate the benefits of different treatment interventions for USN.
Results Table
View results tableOutcomes
Acute phase
Subacute phase
Chronic phase
Phase of stroke recovery not specific to one period
Clinician How-To
Unilateral spatial neglect (USN) e-learning module
Please visit our USN e-learning module: http://elearning.strokengine.org/module.php
What is USN?
Unilateral spatial neglect (USN) is most typically characterized by the inability to orient or respond to stimuli appearing on the contralateral side/hemispace of the brain lesion. Terms including unilateral neglect, hemi-inattention, visual neglect and hemi-spatial neglect are used to describe USN. Over 30% of patients will have post-stroke USN. USN is more frequent in those with a right hemisphere stroke, such that symptoms of USN commonly appear on the left hemispace. Research has shown that damage to the following brain areas leads to USN: right parieto-temporal junction, the angular gyrus, the right inferior parietal lobe, the parahippocampal region and the right superior temporal cortex. Depending on the brain area affected, there are three different types of USN and patients can have one or a combination of the three types with varying degrees of severity:
Personal neglect: Neglect of one side of his/her body (e.g. patients shave/apply makeup to half of their face, usually the left half); acquired from damage to the parietal lobe (post-central and supramarginal gyri);
Near extrapersonal neglect: Neglect of the environment within reaching distance (e.g. patients ignore food on one side of the plate, usually the left half);
Far extrapersonal neglect: Neglect of the space beyond reaching distance (e.g. patients collide into their surroundings, usually the left, when trying to wheel a wheelchair).
*Extrapersonal neglect arises from damage to the frontal lobe (ventral premotor and dorsolateral prefrontal cortex) and the temporal lobe (middle and anterior superior temporal gyrus, and the superior temporal sulcus).
Why is it critical to assess for USN?
Patients with USN are at an increased risk for falls and related injuries, usually have longer rehabilitation stays as well as poorer functional recovery post-stroke. Given that USN can result in falls and lack of independence in daily activities, and that it is treatable, all patients must be quickly screen or assessed for USN during the acute phase post-stroke. Patients identified with the presence of USN must receive effective interventions aimed at reducing impairment and maximizing function.
Who should be assessed?
Perceptual deficits, including USN, are more common in individuals with right hemisphere lesions (RHD). Thus, routine screening for USN in those with RHD is very important. Research has shown that the left hemisphere modulates arousal and attention for the right visual field, whereas the right hemisphere controls these processes in both right and left visual fields. This may be a partial explanation for why USN is not typical in persons with left hemisphere damage (LHD); the intact right hemisphere is capable of compensating for perceptual deficits that result from LHD7. It also substantiates why individuals with RHD experience more severe and longer lasting symptoms of USN compared to those with LHD. The Opponent–processor model argues that each hemisphere attends to the contralateral visual hemispace by inhibiting the other hemisphere. It goes on to propose that with a right hemisphere lesion the left hemisphere is not inhibited, and this results in exaggerated attentional shift to the right (i.e. left USN). USN continues to be commonly associated with a right stroke, but evidence from the literature suggests that all patients with stroke might benefit from USN screening.
Can USN be treated?
Yes, below is an overview of four different types of treatment categories that exist for USN:
- Visual Scanning: The patient with USN is encouraged to explore the neglected visual field (usually the left side) by performing tasks on that side. The treatment often includes a visual target that the patient uses as an anchor while scanning.
- Sensory Stimulation: The therapist uses various types of sensory stimulation to encourage the patient to pay attention to their neglected side. These include:
- Visual/Verbal/Auditory Cues: The use of a visual cue (i.e. red tape or flashing lights), verbal cue (i.e. the voice of the therapist or a family member) or auditory cue (i.e. horn or bell) on the neglected side to improve awareness of that space.
- Limb Activation: The patient actively moves their arm/hand on the neglected side to encourage scanning of that space (usually the left upper extremity towards the left). The patient receiving treatment can do these movements alone or with help from the therapist.
- Caloric Stimulation: The therapist uses a syringe to put either cold or warm water into the patient’s ear (external ear canal) to encourage scanning of the neglected side. Cold water seems to encourage scanning toward the stimulated ear. Warm water encourages scanning of the field opposite to the stimulated ear.
- Eye Patching/Hemiglasses: This treatment uses standard eyeglass frames with either monocular patches (entire eye) or half of both lenses blacked out on the same side (usually the right half). This forces the patient to look through the side of the lens and scan the neglected side (usually the left side).
- Fresnel Prisms: This treatment involves placing prisms over regular eyeglass frames which cause a shift of the visual field. If there is neglect on the left side, these prisms will cause what is seen on the left to be shifted to the right to encourage visual scanning of the left visual field.
- Neck/Hand Vibration or Stimulation: Vibration or stimulation is applied to the side of the neck or hand affected by USN to encourage scanning of the neglected side.
- Trunk Rotation: This strategy involves twisting the trunk toward the neglected side in order to improve visual scanning and awareness of that hemispace.
- Visuo-motor Imagery: Visual imagery involves mental tasks where the patient is required to describe details of a familiar room, environment, or geographic area from their memory. Motor imagery consists of the patient imagining a body movement or posture and describing this sequence. This type of imagery treatment may stimulate areas of the brain that can activate those actual movements during daily activities in order to improve neglect symptoms.
- Constraint-Induced Movement Therapy: This treatment involves restraining the unaffected arm with a sling in order to encourage use of the affected arm. While used primarily to encourage motor return in the affected arm, this intervention will also encourage visual scanning of the patient’s neglected side.
- Optokinetic Stimulation: This involves observation of moving visual targets from left to right, in order to encourage visual scanning of the neglected side
- Video Feedback: This treatment involves filming the patient while he/she does specific activities. The therapist and patient then watch the video together. The therapist points out to the client how they are neglecting their body or the space on the side of their body. They then discuss strategies to encourage the patient to attend to their body and their neglected hemispace.
- Pharmacological Therapy: This involves the use of specific medications (dopamine-agonist drugs) to improve visual attention skills. A physician must prescribe these medications.
Which types of treatments are most effective for post-stroke USN?
The benefits of various interventions to treat post-stroke USN symptoms have been carefully studied.
| Treatment type | Effective (Yes/No) | Level of Evidence |
| Prisms | Yes | Strong (1a) |
| Eye patching | Yes | Limited (2a) |
| Trunk rotation | Yes | Limited (2a) |
| Limb activation | Yes | Limited (2a) |
| Visual-motor imagery | Yes | Limited (2b) |
| Neck/Hand Vibration | Yes | Consensus (3) |
| Caloric Stimulation | Yes | Consensus (3) |
| Visual scanning | Unsure | Conflict (4) |
| Verbal/Visual/Auditory Cues | No | Limited (2a) |
| Optokinetic Stimulation | No | Limited (2a) |
The other treatments methods described in the section above such as constraint-induced movement therapy, video feedback and pharmacological therapy require further research before their effectiveness can be confirmed.
How are these USN treatments administered?
Fresnel Prisms:
To administer fresnel prism therapy, the patient must wear the prisms (deviates their visual field 10º to the right) on their glasses or on goggles. Next, the therapist must engage the patient in a visual scanning task where they repetitively point or reach for two different targets located at each side of their field of vision. According to the studies, the intensity of repetitions varied from 30 to 100 per treatment. The frequency of treatment also varied from 5 sessions of 10 minutes over 2 weeks, to two 20 minute treatments per day for 2 weeks or 30 minutes of scanning performed daily, 5 times per week for 2 weeks.
Eye Patching:
To administer eye patching treatment, the therapist must apply right half patches to both lenses of the patient’s glasses or on goggles for those who do not wear glasses. Patients should wear the glasses/goggles during their waking hours and while doing all tasks. Duration of the eye patching treatment varied from 1 week to 3 months with improved results according to the length of time worn.
Trunk Rotation:
Trunk rotation treatments require the use of a thoracolumbosacral orthosis (e.g. Bon Saint Come’s device) to which a metal bar is attached. The bar is designed to project forward horizontally just above the patients head. The therapist then sets up some visual targets on the patient’s neglected side and asks the patient to repetitively rotate their body towards the target and touch it with the metal bar. This encourages visual scanning of the neglected area. The movements can be performed in a seated or standing position. In the study of the effectiveness of this intervention, patients received 1 hour of trunk rotation per day, every week day for 1 month (total of 20 hours).
Visual/Motor Imagery:
In visual imagery, the therapist guides the patient to mentally visualize scenes that encourage scanning of all areas including the neglected side. For example, the patient imagines that they are a lighthouse and their eyes are the sweeping light at the top scanning the surrounding area. Or, the patient describes a specific room or geographical area. For the motor imagery tasks, the patient is asked to imagine specific postures which they later have to reproduce, as well as specific sequences of movements that would involve the right arm followed by the left arm. Treatment intensities and frequencies ranged from three 30-minute sessions per week for an average of 3 weeks to 40 trials of 50 minute sessions.
Limb Activation:
For limb activation, the therapist instructs the patient to actively move their upper extremity on the neglected side. The therapist can provide verbal or physical cues to guide the patient during this task. The goal is to use active voluntary movements of the upper extremity to promote scanning of the neglected hemispace. For example, the patient can repetitively lift a rod on the left side or displace cones from the right to the left side. Recommended frequency of limb activation therapy is 1 hour per day, for 10 days over a 2-week period.
Visual Scanning:
Visual scanning treatment involves a wide range of activities that encourage the patient to attend to their neglected side. Therapists can engage patients in reading, copying, describing figures or scenes, computer tasks (finding digits on the screen) etc. All of the studies agreed upon an intensity and frequency of 1 hour of treatment per day on a daily basis (5 days per week). However, duration varied from 2, 4 or 8 weeks of treatments. Positive effects of the visual scanning treatments did not increase according to the duration of treatments.
When is the best time to receive treatments for USN?
USN interventions can be provided during the acute, sub-acute, and chronic stages post-stroke.
What type of client is USN treatment for?
USN treatments can be offered to individuals of all ages but should be tailored to the client’s specific level of functioning. Clients with either mild or no cognitive deficits can benefit from therapy (i.e. score ≥22 on the Mini-Mental State Examination is recommended) as they must be able to follow simple commands. Clients must have receptive language abilities in order to be able to understand instructions; however expressive language is not a requirement. Last, patients may have other post-stroke visual impairments such as hemianopsia and it is important o differentiate between the two when assessing treatment benefits.
Who offers these treatments?
Occupational therapists (OTs) typically assess for and provide treatment for USN in an acute care hospital, rehabilitation center, or private clinic.
Special considerations for OTs
There are minimal equipment costs (e.g. prism therapy, eye patching, limb activation) and training required for providing USN treatments. Therapists need to consider that clients with USN may be unable to attend to either one side of his/her body (personal neglect), the space within reaching distance (near extrapersonal neglect), the space beyond reaching distance (far extrapersonal neglect), or to a combination of these three spaces in their environment. Therefore the assessment and treatment of USN within these hemispaces must be considered. It is also important to explain to the patient and their family what USN is and to provide them with safety recommendations such as remembering to put on the wheelchair brake on the left side, and ensuring that the patient does not trip over obstacles on the left. Therapists can also engage the family members aiding with therapy by instructing them to allow the patient to search and find objects in their room which are located on the left side instead of placing all objects within the patient’s field of view.
Screening Tool Administration Procedures
Comb and Razor Test: Patients are required to groom themselves using common objects. For males, this consists of combing and mock shaving (shaving with a shield on) each for 30 seconds. Female patients are asked to comb and demonstrate the use of a facial compact for 30 seconds each. During the 30 second intervals, the evaluator categorizes each “stroke” or touch as having occurred on the left side of the head, the right side of the head, or as ambiguous.
To score the test, observational data is plugged into a formula (% left = left strokes/total strokes x 100), which yields a % value. This value indicates the degree to which the individual being tested has neglected the left side of their head. Left personal neglect is diagnosed when an individual’s mean% left score is less than 35%. The test takes approximately 5 minutes and requires no specialized training to administer.
Albert’s Test: Patients are required to cross through the center of 41 randomly oriented lines, each about 2 cm long, arranged on a sheet of paper. The test sheet is presented to the patient at their midline. The examiner asks the patient to cross out all of the lines, and demonstrates what is required by crossing out the 5 central lines him/herself. The patient is encouraged to cross out all the lines until he/she is satisfied that they have all been crossed.
The presence or absence of USN is based on the number of lines left uncrossed on each side of the test sheet. If any lines are left uncrossed, and more than 70% of uncrossed lines are on the same side as the brain lesion or motor deficit, USN is suspected. This may be quantified in terms of the percentage of lines left uncrossed. The test takes approximately 5 minutes and requires no specialized training to administer.
Baking Tray Task: This test requires that the patient pick-up 16 “buns” and spread them as evenly as possible on a 75×100 cm board. Cubes can be used to represent the “buns”. The therapist must note how the “buns” are spread out and USN can be easily detected depending on their arrangement on the board (i.e. if they are placed on the right side of the board only, left USN is suspected). Patients do not usually exceed 3-5 minutes to complete the task and no specialized training is required to administer the test.
Balloons Test: This bedside test was developed to screen for USN and contains 2 subtests. Subtest A requires the client to cross out the 22 target balloons of the 202 circles that appear on a page within the fixed time limit of 3 minutes. In subtest B, the number and position of balloons is exactly reverse from subtest A, where the client is asked to cross out 10 target circles from the 90 balloons that appear on a page within the fixed time limit of 3 minutes. No specialized training is required to administer the test.
Bells Test: In the Bells Test, the patient is asked to circle with a pencil all 35 bells embedded within 280 distracters (houses, horses, etc.) on an 11 x 8.5 – inch page. The objects are actually equally distributed in 7 columns containing 5 targets and 40 distracters each. Of the 7 columns, 3 are on the left side of the sheet, 1 is in the middle, and 3 are on the right. To administer the test, the examiner must sit facing the patient and place the page at the patient’s midline. The examiner gives the following instructions: “Your task will consist of circling with the pencil all the bells that you will find on the sheet that I will place in front of you without losing time. You will start when I say “go” and stop when you feel you have circled all the bells. I will also ask you to avoid moving or bending your trunk if possible.” If the patient stops before all the bells are circled, the examiner gives only one warning by saying “are you sure all the bells are now circled? Verify again.”
To score the Bell’s test, the total number of circled bells is recorded as well as the time taken to complete. The maximum score is 35. An omission of 6 or more bells on the right or left half of the page indicates USN. Judging by the spatial distribution of the omitted targets, the evaluator can then determine the severity of the visual neglect and the hemispace affected (i.e. left or right).
Clock Drawing Test (CDT): There are a few variations to the CDT:
Free drawn clock: The individual is given a blank sheet of paper and asked first to draw the face of a clock, place the numbers on the clock, and then draw the hands to indicate a given time. To successfully complete this task, the patient must first draw the contour of the clock, then place the numbers 1 through 12 inside, and finally indicate the correct time by drawing in the hands of the clock. A markedly abnormal clock is an important indication that the individual may have a cognitive deficit, warranting further investigation.
Pre-drawn clock: Alternatively, some clinicians prefer to provide the individual with a pre-drawn circle and the patient is only required to place the numbers and the hands on the face of the clock.
Copying a clock: The individual is given a fully drawn clock with a certain time pre-marked and is asked to replicate the drawing as closely as possible. The successful completion of the copy command requires less use of language and memory functions but requires greater reliance on visuospatial and perceptual processes.
Clock reading test: A modified version of the copy command CDT simply asks the patient to read aloud the indicated time on a clock drawn by the examiner.
The time setting “10 after 11” is an ideal setting as it forces the patient to attend to both sides of the clock and requires the recoding of the command “10” to the number “2” on the clock.
The scores are used to evaluate any errors or distortions such as neglecting to include numbers, putting numbers in the wrong place, or having incorrect spacing. Scoring systems may be simple or complex, quantitative or qualitative in nature. The CDT should take approximately 1-2 minutes to complete and requires no specialized training to administer.
Double Letter Cancellation Test (DLCT): The patient is asked to put a mark through all the letters C and E on presented 105 times a sheet of paper containing 6 lines with 52 letters per line. To begin the DLCT, the therapist places the test sheet at the patient’s midline, secures it with tape, and points to the trial line, asking the patient to mark the Cs and Es. If the patient is unable to perform the trial, further instruction is given. If the trial is correctly performed, the therapist will then proceed to give instructions as follows: “Look at the letters on this page. Put one line through each C and E. Ready, begin here”. The therapist points to the first letter in the first row. The time taken to complete the test is recorded.
The score is calculated by subtracting the number of omissions (Cs and Es that were not crossed out) from the possible perfect score of 105. Higher scores indicate better performance. The timing and total number of errors should be noted. The test requires less than 5 minutes to complete and requires no specialized training to administer.
Draw-A-Man Test: This test was initially designed to measure intelligence levels in children, however, has good reliability in detecting USN. To administer the test, the therapist asks the patient to complete three individual drawings (draw a man, a woman, and themselves) on separate pieces of paper. No further instructions are given. There is no right or wrong type of drawing, although the patient must make a drawing of a whole person each time – i.e. head to feet, not just the face. The test has no time limit, however, it is rare that someone takes longer than 10 or 15 minutes to complete all three drawings. Specific scoring instructions for USN can be found in an article by Chen-Sea MJ. Validating the Draw-A-Man Test as a personal neglect test. Am J Occup Therap. 2000;54:391–397.
Line Bisection Test: This is a quickly administered test that requires the patient to mark a line through the center of a series of 17 horizontal lines on an 11x 8.5-inch page. The test is scored by measuring the deviation of the bisection (in centimetres or millimetres) from the true center of the line. A deviation of more than 6 mm from the midpoint indicates USN.
Most testers utilize a formula that divides the deviation by half the length of the line and then multiplies this quotient by 100 to yield a percentage. Omission of two or more lines on one half of the page indicates USN. This test takes less than 5 minutes to complete and requires no specialized training to administer.
Single Letter Cancellation Test: The test consists of one 8.5″x11″ sheet of paper containing 6 lines with 52 letters per line. The stimulus letter “H” is presented 104 times. The page is placed at the patient’s midline. The therapist instructs the patient to put a line through each “H” that is found on the page. The time taken to complete the test is recorded.
The score is calculated by subtracting the number of omissions (H’s that were not crossed out) from the possible perfect score of 104 (0 to 53 on the left and 0 to 51 on the right). Higher scores indicate better performance. Presence of USN can be inferred by calculating the frequency of errors to the left or to the right from the center of the page. Omissions of 4 or more on one side have been found to be pathological.
Star Cancellation Test (SCT): In the Star Cancellation Test, the patient must cross out 56 small stars which are interspersed with 52 large stars, 13 letters, and 10 short words on a sheet of paper. Two small stars in the centre are used for demonstration. The therapist must place the page at the patient’s midline.
The maximum score that can be achieved on the test is 54 points (56 small stars in total minus the 2 used for demonstration). A cut-off of < 44 indicates the presence of USN. A Laterality Index or Star Ratio can be calculated from the ratio of stars cancelled on the left of the page to the total number of stars cancelled. Scores between 0 and 0.46 indicate USN in the left hemispace. Scores between 0.54 and 1 indicate USN in the right hemispace. The test takes under 5 minutes to administer and requires no specialized training for the tester.
National Institute of Health Stroke Scale (NIHSS): The NIHSS is a 15-item impairment scale, intended to evaluate neurologic outcome and degree of recovery for patients with stroke. The scale assesses various outcomes with the one item involving the assessment of USN for the personal space and near extrapersonal space. There are no specific instructions for assessing USN, however, the test states that sufficient information to detect neglect may be obtained from testing the prior items and is rated from 0 – 2.
Short Version – Rivermead Behavioral Inattention Test (RBIT): The short version of the RBIT involves three conventional subtests (line crossing, Star Cancellation Test, and figure copying) and five behavioural subtests (scanning a picture, reading a menu, eating a meal, reading an article, and sorting coins). Administration procedures and scoring methods can be found in the RBIT manual.
Semi-Structured Scale for the Functional Evaluation of Hemi-inattention in Extrapersonal Space: Patients are asked to perform different tasks with real objects. To assess personal neglect, patients must demonstrate the use of three common objects: comb, razor/powder compact, and eyeglasses. The objects are placed at the patient’s midline one at a time and he/she is asked to demonstrate how each are used. To assess extrapersonal neglect, patients must serve tea, deal cards, describe a picture, and describe an environment.
- Serving tea:
The patient is brought to a table with a tray containing 4 cups and saucers, a teapot, a sugar bowl, teaspoons, and paper napkins. Examiners are seated both on the right, in front, and to the left of the patient who is asked to serve tea for him/herself and for those who are with him/her, to distribute napkins and teaspoons, and also to serve the sugar. The examiner, who is seated in front of the patient asks: “Would you like to serve the tea?”. If the patient serves the tea but not the napkins and/or teaspoons, the examiner asks: “Would you like to give us the teaspoons (napkins)?”. - Card dealing.
The examiners and the patient are seated the same way as they were for the tea-serving situation. The patient is asked if he/she knows how to play “Scopa”. If necessary, he/she is reminded of the basic rules (3 cards for each player and 4 in the middle of the table). The examiner seated in front of the patient asks: “Would you like to deal the cards for a game of Scopa?”. - Picture description.
A picture is placed in front of the patient and he/she is asked: “Will you describe everything you see in this picture?”. Three pictures are used. Two are cards 3 and 6 of Set 1 of the Progressive Picture Compositions by Byrne (1967); one is Tissot’s painting ‘The dance on the ship’. The examiner indicates the persons and objects pointed out by the patient with progressive numbers on a photocopy of the stimulus figure in the order in which they are reported, without soliciting in any way. - Description of an environment.
The patient is placed in a room full of objects on both sides (arm chairs, pictures, lamps) and is asked to describe it. The patient is told: “Will you describe everything you see in this room?”. To facilitate scoring, it is useful to record the elements described by the patient on a schematic drawing of the environment.
Info Pocket Booklet
References
- Antonucci, G., Guariglia, C., Judica, A., Magnotti, L., Paolucci, S., Pizzamiglio, L., & Zoccolotti, P. (1995). Effectiveness of neglect rehabilitation in a randomized group study.Journal of Clinical and Experimental Neuropsychology, 17(3), 383-9. http://www.ncbi.nlm.nih.gov/pubmed/7650101
- Bailey, M.J., Riddoch, M.J., & Crome, P. (2002). Treatment of visual neglect in elderly patients with stroke
Also called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain.: a single-subject series using either a scanning and cueing strategy or a left-limb activation strategy.Physical Therapy, 82(8), 782-797. http://www.ncbi.nlm.nih.gov/pubmed/12147008 - Beis, J.M., A, J.M., Baumgarten, A., & Challier, B. (1999). Eye patching
A form of intervention that involves placing one right monocular patch or two right half-field patches on a pair of standard eyeglass frames. For persons with USN, eye patching conceals the visual field of the non-affected side in order to encourage visual scanning of the neglected hemispace.
in unilateral spatial neglect: Efficacy of two methods.Archives of Physical Medicine and Rehabilitation, 80, 71-6. http://www.ncbi.nlm.nih.gov/pubmed/9915375 - Cazzoli, D., Mur, R.M., Schumacher, R., von Arx, S., Chaves, S., Gutbrod, K., Bohlhalter, S., Bauer, D., Vanbellingen, T., Bertschi, M., Kipfer, S., Rosenthal, C.R., Kennard, C., Bassetti, C.L., & Nyffeler, T. (2012). Theta burst stimulation
3 bursts of transcranial magnetic stimulation at 50Hz and repeating at 5Hz at 80% of resting motor threshold.
reduces disability during the activitiesAs defined by the International Classification of Functioning, Disability and Health, activity is the performance of a task or action by an individual. Activity limitations are difficulties in performance of activities. These are also referred to as function.
of daily living in spatial neglect.Brain, 135, 3426-3439. http://www.ncbi.nlm.nih.gov/pubmed/22831781 - Dohle, C., Püllen, J., Nakaten, A., Küst, J., Rietz, C., & Karbe, H. (2009). Mirror therapy promotes recovery from severe hemiparesis: a randomized controlled trial. Neurorehabilitation and Neural Repair, 23, 209-217. http://www.ncbi.nlm.nih.gov/pubmed/19074686
- Fanthome, Y., Lincoln, N.B., Drummond, A., & Walker, M.F. (1995). The treatment of visual neglect using feedback of eye movements: a pilot study.Disability and Rehabilitation, 17(8), 413-417. http://www.ncbi.nlm.nih.gov/pubmed/8573702
- Ferreira, H.P., Lopes, M.A.L., Luiz, R.R., Cardosa, L., & Andre, C. (2011). Is visual scanning
During this intervention the person with USN is encouraged to conduct voluntary eye movements toward the neglected visual field (usually the left side) by performing a task in that hemispace. The treatment often includes a visual target that the patient uses as an anchor to direct voluntary gaze control while scanning.
better than mental practice in hemispatial neglect? Results from a pilot study.Topics in StrokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. Rehabilitation, 18(2), 155-161. http://www.ncbi.nlm.nih.gov/pubmed/21447465 - Fong, K.N.K., Yang, N.Y.H., Chan, M.K.L., Chan, D.Y.L., Lau, A.F.C., Chan, D.Y.W., Cheung, J.T.Y., Cheung, H.K.Y., Chung, R.C.K., & Chan, C.C.H. (2013). Combined effects of sensory cueing and limb activation
A form of intervention that involves voluntary movement of the arm and hand. For persons with USN, voluntary movements of the affected upper extremity on the neglected side can encourage visual scanning and exploration of that hemispace.
on unilateral neglect in subacute left hemiplegic strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. patients: a randomized controlled pilot study.Clinical Rehabilitation, 27(7), 628-37. http://www.ncbi.nlm.nih.gov/pubmed/23405025 - Frassinetti, F., Angeli, V., Meneghello, F., Avanzi, S., & Ladavas, E. (2002). Long-lasting amelioration of visuospatial neglect by prism adaptation.Brain, 125, 608-623. http://www.ncbi.nlm.nih.gov/pubmed/11872617
- Harvey M., Hood B., North A., & Robertson I. (2003). The effects of visuomotor feedback training on the recovery of hemispatial neglect symptoms: assessment of a 2-week and follow-up intervention.Neuropsychologia, 41, 886-93. http://www.ncbi.nlm.nih.gov/pubmed/12667525
- Ianes, P., Varalta, V., Gandolfi, M., Picelli, A., Corno, M., Di Matteo, A., Fiaschi, A., & Smania, N. (2012). Stimulating visual exploration of the neglected space in the early stage of stroke
Also called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. by hemifield eye-patching: a randomized controlled trial in patients with right brain damage.European Journal of Physical Rehabilitation and Medicine, 48, 189-96. http://www.ncbi.nlm.nih.gov/pubmed/22083263 - Jo, K., Yu, J., & Jung, J. (2012). Effects of virtual reality-based rehabilitation on upper extremity function and visual perception in stroke
Also called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. patients: A randomized control trial.Journal of Physical Therapy Science, 24, 1205-1208. - Kalra, L., Perez, I., Gupta, S., & Wittink, M. (1997). The influence of visual neglect on stroke
Also called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. rehabilitation.Stroke Also called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain., 28(7), 1386-91. http://www.ncbi.nlm.nih.gov/pubmed/9227688 - Kamada, K., Shimodozono, M., Hamada, H., & Kawahira, K. (2011). Effects of 5 minutes of neck-muscle vibration immediately before occupational therapy on unilateral spatial neglect.Disability and Rehabilitation, 33(23-24), 2322-28. http://www.ncbi.nlm.nih.gov/pubmed/21486139
- Katz, N., Ring, H., Naveh, Y., Kizony, R., Feintuch, U., Weiss, P.L. (2005). Interactive virtual environment training for safe street crossing of right hemisphere stroke
Also called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. patients with Unilateral Spatial Neglect.Disability and Rehabilitation, 27(20), 1235-43. http://www.ncbi.nlm.nih.gov/pubmed/16298925 - Kerkhoff, G., Keller, I., Artinger, F., Hildebrandt, H., Marquardt, C., Reinhart, S., & Ziegler, W. (2012). Recovery from auditory and visual neglect after optokinetic stimulation
A form of intervention for USN that involves the observation of moving visual targets to encourage visual scanning of the neglected hemispace. A computer screen is typically used to display a leftward moving background of dots or strips in order to produce the illusions of visual stimuli being displaced to the right.
with pursuit eye movements – transient modulation and enduring treatment effects.Neuropsychologia, 50, 1164-1177. http://www.ncbi.nlm.nih.gov/pubmed/21964557 - Kim, B.R., Chun, M.H., Kim, D-Y., & Lee, S.J. (2013). Effect of high- and low-frequency repetitive transcranial magnetic stimulation on visuospatial neglect in patients with acute stroke
Also called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain.: a double-blind, sham-controlled trial.Archives of Physical Medicine and Rehabilitation, 94, 803-7. http://www.ncbi.nlm.nih.gov/pubmed/23298790 - Kim, Y.M., Chun, M.H., Yun, G.J., Song, Y.J., & Young, H.E. (2011). The effects of virtual reality training on unilateral spatial neglect in stroke
Also called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. patients.Annals of Rehabilitation Medicine, 35, 309-15. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3309210/ - Koch, G., Bonni S., Giacobbe, V., Bucchi, G., Basile, B., Lupo, F., Versace, V., Bozzali, M., & Caltagirone, C. (2012). Theta-burst stimulation of the left hemisphere accelerates recovery of hemispatial neglect.Neurology, 78, 24-30. http://www.ncbi.nlm.nih.gov/pubmed/22170878
- Ladavas, E., Menghini, G., & Umilta, C. (1994). A rehabilitation study of hemispatial neglect.Cognitive Neuropsychology, 11(1), 75-95. http://www.tandfonline.com/doi/abs/10.1080/02643299408251967#.VmCNJtIvfs0
- Luukkainen-Markkula, R., Tarkka, I.M., Pitkanen, K., Sivenius, J., & Hamalainen, H. (2009). Rehabilitation of hemispatial neglect: A randomized study using either arm activation or visual scanning
During this intervention the person with USN is encouraged to conduct voluntary eye movements toward the neglected visual field (usually the left side) by performing a task in that hemispace. The treatment often includes a visual target that the patient uses as an anchor to direct voluntary gaze control while scanning.
training.Restorative Neurology and Neuroscience, 27, 665-674. http://www.ncbi.nlm.nih.gov/pubmed/20042790 - Mancuso, M., Pacini, C., Gemignani, P., Bartalini, B., Agostini, B., Ferroni, L., Caputo M., Capitani, D., Mondin, E., & Cantagallo, A. (2012). Clinical application of prismatic lenses in the rehabilitation of neglect patients. A randomized controlled trial.European Journal of Physical Rehabilitation and Medicine, 48, 197-208. http://www.ncbi.nlm.nih.gov/pubmed/22318363
- Mizuno, K., Tsuji, T., Takebayashi, T., Fujiwara, T., Hase, K., & Liu, M. (2011). Prism adaptation therapy enhances rehabilitation of stroke
Also called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. patients with unilateral spatial neglect: a randomized, controlled trial.Neurorehabilitation and Neural Repair, 25(8), 711-20. http://www.ncbi.nlm.nih.gov/pubmed/21700922 - Modden, C., Behrens, M., Damke, I., Eilers, N., Kastrup, A., & Hildebrandt, H. (2012). A randomized controlled trial comparing 2 interventions for visual field loss with standard occupational therapy during inpatient stroke
Also called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. rehabilitation.Neurorehabilitation and Neural Repair, 26(5), 463-9. http://www.ncbi.nlm.nih.gov/pubmed/22140199 - Niemeier, J.P., Cifu, D.X., & Kishore, R. (2001). The lighthouse strategy: improving the functional status of patients with unilateral neglect after stroke
Also called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. and brain injury using a visual imagery intervention.Topics in Stroke Also called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. Rehabilitation, 8(2), 10-18. http://www.ncbi.nlm.nih.gov/pubmed/14523742 - Nijboer, T.C.W., Olthoff, L., Van der Stigchel, S., & Visser-Meily, J.M.A. (2014). Prism adaptation improves postural imbalance in neglect patients.NeuroReport, 25, 307-11. http://www.ncbi.nlm.nih.gov/pubmed/24488029
- Nys, G.M.S., De Haan, E.H.F., Kunneman, A., De Kort, P.L.M., & Dijkerman, H.C. (2008). Acute neglect rehabilitation using repetitive prism adaptation: A randomized placebo-controlled trial. Restorative Neurology and Neuroscience, 26(1), 1-12. http://www.ncbi.nlm.nih.gov/pubmed/18431002
- Osawa, A. & Maeshima, S. (2010). Family participation
As defined by the International Classification of Functioning, Disability and Health, participation is an individual's involvement in life situations in relation to health conditions, body functions or structures, activities, and contextual factors. Participation restrictions are problems an individual may have in the manner or extent of involvement in life situations. can improve unilateral spatial neglect in patients with acute right hemispheric stroke Also called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain..European Neurology, 63, 170-175. http://www.ncbi.nlm.nih.gov/pubmed/20185919 - Pandian, J.D., Arora, R., Kaur, P., Sharma, D., Vishwambaran, D.K., Arima, H. (2014). Mirror therapy in unilateral neglect after stroke
Also called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain..Neurology, 83, 1-6. http://www.ncbi.nlm.nih.gov/pubmed/25107877 - Paolucci, S., Antonucci, G., Guariglia, C., Magnotti, L., Pizzamiglio, L., & Zoccolutti, P. (1996). Facilitatory effect of neglect rehabilitation on the recovery of left hemiplegic stroke
Also called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. patients: a cross-over study.Journal of Neurology, 243, 308-14. http://www.ncbi.nlm.nih.gov/pubmed/8965102 - Pisella L, Rode G, Farnè A, Boisson D, Rossetti Y. (2002). Dissociated long lasting improvements of straight-ahead pointing and line bisection tasks in two hemineglect patients. Neuropsychologia.;40(3):327-34.http://www.ncbi.nlm.nih.gov/pubmed/11684165
- Pizzamiglio, L., Fasotti, L., Jehkonen, M., Antonucci, G., Magnotti, L., Boelen, D., & Sanna, A. (2004). The use of optokinetic stimulation
A form of intervention for USN that involves the observation of moving visual targets to encourage visual scanning of the neglected hemispace. A computer screen is typically used to display a leftward moving background of dots or strips in order to produce the illusions of visual stimuli being displaced to the right.
in rehabilitation of the hemineglect disorder.Cortex, 40, 441-450. http://www.ncbi.nlm.nih.gov/pubmed/15259325 - Polanowska, K., Seniow, J., Paprot, E., Lesniak, M., & Czlonkowska, A. (2009). Left-hand somatosensory stimulation combined with visual scanning
During this intervention the person with USN is encouraged to conduct voluntary eye movements toward the neglected visual field (usually the left side) by performing a task in that hemispace. The treatment often includes a visual target that the patient uses as an anchor to direct voluntary gaze control while scanning.
training in rehabilitation for post-stroke hemineglect: A randomised, double-blind study. Neuropsychological Rehabilitation, 19(3), 364-382. http://www.ncbi.nlm.nih.gov/pubmed/18663642 - Robertson, I.H., Gray, J.M., Pentland, B., & Waite, L.J. (1990). Microcomputer-based rehabilitation for unilateral left visual neglect: a randomized controlled trial.Archives of Physical Medicine and Rehabilitation, 71, 663-8. http://www.ncbi.nlm.nih.gov/pubmed/2375671
- Robertson, I.H., McMillan, T.M., MacLeod, E., Edgeworth, J., & Brock, D. (2002). Rehabilitation by limb activation
A form of intervention that involves voluntary movement of the arm and hand. For persons with USN, voluntary movements of the affected upper extremity on the neglected side can encourage visual scanning and exploration of that hemispace.
training reduces left-sided motor impairmentLoss of strength and coordination, decrease in arm or leg movement
in unilateral neglect patients: a single-blind randomised control trial.Neuropsychological Rehabilitation, 12(5), 439-54. http://www.tandfonline.com/doi/abs/10.1080/09602010244000228 - Rorsman, I. & Johansson, B. (2006). Can electro-acupuncture or transcutaneous nerve stimulation influence cognitive and emotional outcome after stroke
Also called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain.?Journal of Rehabilitation Medicine, 38, 13-19. http://www.ncbi.nlm.nih.gov/pubmed/16548081 - Rossetti, Y., Rode, G., Pisella, L., Farne, A., Boisson, D., & Perenin, M.T. (1998). Prism adaptation to a rightward optical deviation rehabilitates left hemispatial neglect.Nature, 395, 166-9. http://www.ncbi.nlm.nih.gov/pubmed/9744273
- Rossi, P.W., Kheyfets, S., & Reding, M.J. (1990). Fresnel prisms
A form of intervention that involves placing prisms over regular eyeglass frames, which result in a shift of the visual field so that visual targets appear deviated from their original position. When wearing the eye glasses patients initially reach toward the virtual position of the target due to their deviated vision. After repeated treatments with Fresnel prisms, patients can correct their visual positioning and will reach the actual target. For persons with USN, prisms may be used to encourage visual scanning of the neglected hemispace.
improve visual perception in strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. patients with homonymous hemianopia or unilateral visual neglect.Neurology, 40(10), 1597-9. http://www.ncbi.nlm.nih.gov/pubmed/2215953 - Schroder, A., Wist, E.R., & Homberg, V. (2008). TENS and optokinetic stimulation
A form of intervention for USN that involves the observation of moving visual targets to encourage visual scanning of the neglected hemispace. A computer screen is typically used to display a leftward moving background of dots or strips in order to produce the illusions of visual stimuli being displaced to the right.
in neglect therapy after cerebrovascular accident: A randomized controlled study.European Journal of Neurology, 15, 922-927. http://www.ncbi.nlm.nih.gov/pubmed/18637956 - Sedda, A., Borghese, N.A., Ronchetti, M., Mainetti, R., Pasotti, F., Beretta, G., & Bottini, G. (2013). Using virtual reality to rehabilitate neglect.Behavioral Neurology, 26, 183-185. http://www.ncbi.nlm.nih.gov/pubmed/22713415
- Serino, A., Barbiani, M., Rinaldesi, L., & Ladavas, E. (2009). Effectiveness of prism adaptation in neglect rehabilitation: A controlled trial study.Stroke
Also called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain., 40, 1-7. http://www.ncbi.nlm.nih.gov/pubmed/19246708 - Turton, A.J., O’Leary, K., Gabb, J., Woodward, R., & Gilchrist, I.D. (2010). A single blinded randomized controlled pilot trial of prism adaptation for improving self-care in stroke
Also called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. patients with neglect.Neuropsychological Rehabilitation, 20(2), 180-196. http://www.ncbi.nlm.nih.gov/pubmed/19629848 - van Kessel, M.E., Geurts, A.C.H., Brouwer, W.H., & Fasotti, L. (2013). Visual scanning
During this intervention the person with USN is encouraged to conduct voluntary eye movements toward the neglected visual field (usually the left side) by performing a task in that hemispace. The treatment often includes a visual target that the patient uses as an anchor to direct voluntary gaze control while scanning.
training for neglect after strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. with and without a computerized lane tracking dual task.Frontiers in Human Neuroscience, 7, 1-11. http://www.ncbi.nlm.nih.gov/pubmed/23847519 - Webster, J.S., McFarland, P.T., Rapport, L.J., Morrill, B., Roades, L.A., & Abadee, P.S. (2001). Computer-assisted training for improving wheelchair mobility in unilateral neglect patients.Archives of Physical Medicine and Rehabilitation, 82, 769-75. http://www.ncbi.nlm.nih.gov/pubmed/11387581
- Weinberg, J., Diller, L., Gordon, W.A., et al. (1977). Visual scanning
During this intervention the person with USN is encouraged to conduct voluntary eye movements toward the neglected visual field (usually the left side) by performing a task in that hemispace. The treatment often includes a visual target that the patient uses as an anchor to direct voluntary gaze control while scanning.
training effect on reading-related in acquired right brain damage.Archives of Physical Medicine and Rehabilitation, 58, 479-86. http://www.ncbi.nlm.nih.gov/pubmed/931586 - Weinberg, J., Diller, L., Gordon, W.A., et al. (1979). Training sensory awareness and spatial organization in people with right brain damage.Archives of Physical Medicine and Rehabilitation, 60, 491-6. http://www.ncbi.nlm.nih.gov/pubmed/508074
- Wiart, L., Bon Saint Come, A., Debelleix, X., Petit, H., Joseph, P.A., Mazaux, J.M., & Barat, M. (1997). Unilateral neglect syndrom rehabilitation by trunk rotation
A form of intervention that involves actively twisting the body's trunk towards the affected side. This can also be performed passively by means of a shoulder strap or corset. For persons experiencing USN, trunk rotation may be used to improve visual scanning and exploration of the neglected hemispace.
and scanning training.Archives of Physical Medicine and Rehabilitation, 78(4), 424-9. http://www.ncbi.nlm.nih.gov/pubmed/9111464 - Zeloni, G., Farne, A., & Baccini, M. (2002). Viewing less to see better.Journal of Neurology, Neurosurgery and Psychiatry, 73(2), 195-8. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1737996/
Exlcuded Studies:
Castiello, U., Lusher, D., Burton, C., et al. (2004). Improving left hemispatial neglect using virtual reality. Neurology, 62, 1958-62.
Reason for exclusion: Feasibility study.
Dick, A. S., Raja Beharelle, A., Solodkin, A., & Small, S. L. (2013). Interhemispheric functional connectivity following prenatal or perinatal brain injury predicts receptive language outcome. J Neurosci., 33(13), 5612-5625.
Reason for exclusion: Study participants were children.
Ertekin, A., Gelecek, N., Yildirim, Y., & Akdal, G. (2009). Supervised versus home physiotherapy outcomes in stroke patients with unilateral visual neglect: a randomized controlled follow-up study. Journal of Neurological Sciences, 26 (3), 325-34.
Reason for exclusion: Both groups were given the same exercise program to target USN, which was then performed under supervision or as a home program.
Hommel, M., Peres, B., Pollak, P., Memin, B., Besson, G., Gaio, J.M., & Perret, J. (1990). Effects of passive tactile and auditory stimuli on left visual neglect. Archives of Neurology, 47, 573-576.
Reason for exclusion: No control group.
Kim, J., Kim, K., Kim, D.Y., Chang, W.H., Park, C., Ohn, S.H., Han, K., Ku, J., Nam, S.W., Kim, I.Y., & Kim, S.I. (2007). Virtual reality training system for rehabilitation of stroke patients with unilateral neglect: crossing the virtual street. CyberPsychology & Behavior, 10(1), 7-15.
Reason for exclusion: Feasibility study.
Tham, K. & Tegner, R. (1997). Video feedback in the rehabilitation of patients with unilateral neglect. Archives of Physical Medicine and Rehabilitation, 78, 410-413.
Reason for exclusion: Both groups received sensory feedback (verbal feedback vs. visual feedback).
Trislin, I., Dupierriz, E., Chokron, S., Coquillart, S., & Ohlmann, T. (2009). Uses of virtual reality for diagnosis, rehabilitation and study of unilateral spatial neglect: review and analysis. CyberPsychology & Behavior, 12(2), 175-81.
Reason for exclusion: Review article.
Walker, R., Young, A.W., & Lincoln, N.B. (1996). Eye patching and the rehabilitation of visual neglect. Neuropsychological Rehabilitation, 6(3), 219-231.
Reason for exclusion: No control group.