Positioning
Introduction
Proper positioning post-stroke is essential in order to reduce the risk of shoulder subluxation, contractures and pain. Proper positioning may also enhance motor recovery, range of motion, and oxygen saturation.
In this module we identify the evidence for optimal positioning of the patient when:
- Lying: supine, on affected side and on non-affected side,
- Sitting: in bed, chair and wheelchair,
- Standing and transferring.
Patient/Family Information
Authors*: Erica Kader; Nicol Korner-Bitensky, PhD OT; Elissa Sitcoff, BA BSc; Leila Goulamhoussen, BSc OT; Rabiaa Laroui, BSc OT; Sheila Liu, BSc OT; Anita Petzold, BSc OT; Anna Rentoulis, BSc OT; Stephen Tang, BSc OT
What is positioning?
After a stroke, muscles can be affected in various ways, causing pain, spasticity, and problems with speed and range of motion. One way to minimize these effects is to properly support, position, and align your body. While in the hospital or rehabilitation centre, your healthcare professional will suggest ways to position your body that are safe and comfortable. This may include the teaching of proper techniques when transferring from sitting to standing, or using devices such as foam wedges or slings to maintain support.
Why is positioning important after a stroke?
Proper positioning can be useful to minimize or prevent pain and stiffness that are commonly present post-stroke. It can also help you to regain movement that was lost after your stroke, or limit future problems with movement. In addition, proper positioning has been shown to increase awareness and protection of the weaker side of the body.
Some common positions recommended following a stroke
- Positioning while lying on your back: Pillows are placed behind the shoulder, head, weaker arm, and hip. The feet are placed in a neutral position.
- Positioning while lying on the weaker side: When lying on the weaker side, one or two pillows are placed under the head, the weaker shoulder is positioned comfortably on a pillow, the stronger leg is forward on one or two pillows, and the weaker leg is straight out. Pillows are also placed in back and in front of the body.
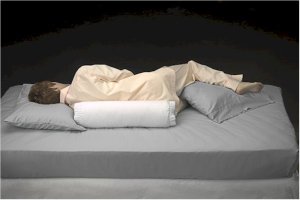
- Positioning while lying on the stronger side: One or two pillows are placed under the head, while the weaker shoulder is placed forward with the weaker arm supported by pillows. The weaker leg is placed toward the back on pillows.
- Positioning while sitting up: The individual is seated at the centre of the chair or wheelchair, their arms placed forward onto pillows on their lap or on a table. Feet are placed flat on the floor or on footrests with knees bent directly above the feet.
- Positioning while sitting in bed: Sitting up in bed is recommended for short periods only as it is better to sit in a chair as soon as possible. The individual will sit upright, well supported by pillows. Arms are placed on pillows on either side of the body and legs are extended comfortably.
- Positioning during transfers: During transfers to a chair or from a chair to another chair, positioning of the weaker shoulder and upper arm is important. The weaker arm should always be supported during transfers, and it is important that no one pull on the arm as it can cause pain in your shoulder that will be difficult to eliminate once created. For getting out of bed, it may be useful to install a bar beside your bed that you can hold onto with your stronger arm to help push yourself up to the standing position.

Photo courtesy of www.invisiblecaregiver.com - Positioning while standing and walking: While standing up and moving around, slings and supports are used for positioning of the weaker arm.
How effective is positioning after stroke?
- Preventing shoulder pain: Arm positioning while lying and sitting was shown to be ineffective in preventing shoulder pain for all stages of stroke. However positioning of the weaker arm using slings and supports while standing and moving around was shown to be effective in preventing shoulder pain. There was no evidence as to whether positioning of the shoulder and arm during transfers was effective in preventing shoulder pain but it is definitely best practice to protect the weaker arm by supporting it (and never pulling on it) during transfers.
- Reducing shoulder pain: Positioning of the weaker shoulder and arm using slings and supports while standing and moving around was shown to be an effective way of reducing shoulder pain. No evidence was found to show that upper limb positioning during transfers would reduce shoulder pain. Arm positioning while lying and sitting was also found to be ineffective in reducing shoulder pain. Again it is important to note that it is definitely best practice to support the weaker arm (and never pull on it) during standing and walking.
- Preventing and reducing shoulder subluxation (dislocation of the shoulder): There is conflicting scientific evidence concerning the effectiveness of arm positioning while sitting on the prevention of shoulder subluxation (dislocation). Upper limb positioning while standing and walking is effective in preventing and reducing shoulder dislocation.
- Improving range of motion: Proper arm positioning while lying and sitting has been shown to be ineffective for improving arm range of motion (how much it can move through space).
- Improving functional independence: Proper arm positioning while lying and sitting has been shown to be ineffective in improving ability to perform daily tasks after a stroke.
- Increasing awareness of the upper limb: No evidence was found concerning the effectiveness of arm positioning while sitting to increase awareness of the weaker arm. Generally, best practice is to have the arm placed in a position where the patient is able to see the arm – for example on a lap tray if the person is sitting in a wheelchair.
What devices can I use for positioning?
Positioning devices exist for various purposes, including support and padding. Below you will find examples of some of the devices that are available to aid in positioning. Your health care provider can give you information on positioning aids that are appropriate for your specific needs.
- Slings: Various slings are available and can be used following a stroke to support your weaker arm while you are standing or during transfers. Slings can prevent pain that is caused by dislocation of the shoulder.

- Head Donut: This supports the back of your head when lying down.

- Pillows: Pillows are used for padding and protection of some pressure points of the arm and legs, such as elbows, knees, and heels.
- Wedges: Wedges are placed under your knees to prevent you from sliding in a chair while sitting down.
- Lap trays: Lap trays are attached to the armrest of a wheelchair and lay across your lap. This will allow you to rest your weaker arm on the tray.
- Arm trough: Arm troughs are placed on the armrest of the wheelchair to keep your weaker arm from hanging over the side. A strap can also be added to the trough to provide additional support.

- Harness: These can be used for the weaker shoulder. They are often adjustable and fastened with Velcro. A shoulder harness offers support by fitting over the weaker shoulder, and passing behind the neck to strap onto the stronger arm.

Where can I get the devices to aid in positioning?
Your healthcare professional will help you to choose the devices that are appropriate for your needs as well as ensure a proper fit. If they cannot supply you with your positioning aids they will direct you to a supplier from whom you can purchase these devices. Be sure to get information from your supplier or healthcare provider on proper cleaning and maintenance of your positioning aid.
How much does it cost?
Positioning devices are available for purchase either from your rehabilitation facility, or directly from the supplying companies themselves. Suppliers range in price. It is possible that your positioning devices may be covered by your health insurance.
Are there any side effects/risks?
There are generally no side effects to proper positioning after a stroke. It is important to consult with a healthcare professional who can give you appropriate advice, since incorrect positioning can put strain on your muscles, cause discomfort, and of course will not give beneficial results.
Who can help me with positioning?
It is important that a trained healthcare professional show you how to properly and safely position your body and upper limb following a stroke. This type of advice is usually provided by a physical or occupational therapist. Your therapist can also teach proper positioning techniques to your family and friends so that they can help you as well.
Clinician Information
Positioning of the upper extremity is used to prevent pain, contractures, and shoulder subluxation and to improve motor recovery, range of motion, and oxygen saturation. We conducted a systematic review of the scientific literature to compile current knowledge regarding the effectiveness of post-stroke positioning.
The results of 17 studies including four high quality RCTs, one quasi experimental study, one case-control study, six repeated-measures studies, and five surveys were compiled to summarize the current knowledge on positioning of patients post-stroke. In addition, references from one review article were retrieved and reviewed to identify any that were research based: all were expert opinion or textbook references rather than study based.
Results Table
View results tableOutcomes
Static arm positioning (without strapping) while lying or sitting – Acute phase
Static arm positioning (without strapping) while lying or sitting – Subacute phase
Static arm positioning (without strapping) while lying or sitting – Chronic phase
Body positioning during lying
Upper extremity positioning in sitting
Upper extremity positioning during transfers
References
- Ada L., Goddard E., McCully J., & Bampton J. (2005). Thirty minutes of positioning reduces the development of shoulder external rotation contracture after stroke: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation, 86(2): 230-34.
- Boyd E.A., Pepin P., & Szabo-Hartin J. (1999). Shoulder supports revisited: A Canadian follow-up survey. Canadian Journal of Occupational Therapy, 66(4): 161-68.
- Brooke M.M., de Lateur B.J., Diana-Rigby C.G., & Questad K.A.(1991). Shoulder Subluxation in Hemiplegia: Effects of Three Different Supports. Archives of Physical Medicine and Rehabilitation, 72: 582-86.
- Carr E.K., & Kenney F.D. (1992). Positioning of the stroke patient: a review of the literature. International Journal of Nursing Studies, 29: 355-369.
- Chatterton H.J., Pomeroy V.M., & Gratton, J. (2001). Positioning for stroke patients: a survey of physiotherapists aims and practices. Disability and Rehabilitation, 23(10), 413-421.
- Chatterton H.J., Pomeroy V.M., Connolly M.J., Faragher E.B., Clayton L., & Tallis, R.C. (2000). The effect of body position on arterial oxygen saturation in acute stroke. Journal of gerontology, 55A(4); M239-M244.
- De Jong L.D., Nieuwboer A., & Aufdemkampe, G. (2006). Contracture preventive positioning of the hemiplegic arm in subacute stroke patients: a pilot randomized controlled trial. Clinical Rehabilitation, 20: 656-667.
- Dean C.M., Mackey F.H., & Katrak P. (2000). Examination of shoulder positioning after stroke: A randomized controlled pilot trial. Australian Journal of Physiotherapy, 46:35-40.
- Elizabeth J., Singarayar J., Ellul J., Barer D., & Lye M. (1993). Arterial oxygen saturation and posture in acute stroke. Age & Ageing, 22(4):269-72.
- Foongchomcheay A., Ada L., & Canning C. (2005). Use of devices to prevent subluxation of the shoulder after stroke. Physiotherapy Research International 10: 134-145.
- Gilmore P.E., Spaulding S.J., & Vandervoort A.A. (2004). Hemiplegic shoulder pain: Implications for occupational therapy treatment. The Canadian Journal of Occupational Therapy, 71(1): 36-46.
- Gustafsson L., & McKenna K. (2006). A program of static positional stretches does not reduce hemiplegic shoulder pain or maintain shoulder range of motion-a randomized controlled trial. Clinical Rehabilitation, 20:277-86.
- Hurd M., Farrel K., &Waylonis G. (1974). Shoulder Sling for Hemiplegia: Friend or Foe? Archives of Physical Medicine and Rehabilitation, 55: 519-522.
- Mee L.Y., & Bee W.H. (2007). A comparison study on nurses’ and therapists’ perception on the positioning of stroke patients in Singapore General Hospital. International Journal of Nursing Practice, 13(4): 209-21
- Mee L.Y., & Bee W.H. (2007). A comparison study on nurses’ and therapists’ perception on the positioning of stroke patients in Singapore General Hospital. International Journal of Nursing Practice, 13(4): 209-21.
- Moodie N.B., Brisnin J., & Morgan A.M.G. (1986). Subluxation of the glenohumeral joint in hemiplegia: Evaluation of supportive devices. Physiotherapy Canada, 38 (3): 151-57.
- Rowat A.M. (2001). What do nurses and therapists think about the positioning of stroke patients? Journal of Advanced Nursing, 34(6): 795-803.
- Seneviratne C., Then K.L., Reimer, M. (2005). Post-stroke shoulder subluxation: a concern for neuroscience nurses. AXON, 27(1): 26-31.
- Wojner A.W., El-Mitwalli A., & Alexandrov A.V. (2002). Effect of Head positioning on intracranial blood flow velocities in acute ischemic stroke: a pilot study. Critical Care Nurse, 24(4): 57-66.
- Wojner A.W., Garami Z., Chenyshev O.Y., & Alexandrov A.V. (2005). Head down: flat positioning improves blood flow velocity in acute ischemic stroke. American Academy of Neurology, 64: 1354-1357.
- Zorowitz R.D., Idank D., Ikai T., Hughes M.B., & Johnson M.V. (1995). Shoulder Subluxation After Stroke: A comparison of four Supports. Archives of Physical Medicine and Rehabilitation, 76: 763-771.



