Line Bisection Test
Purpose
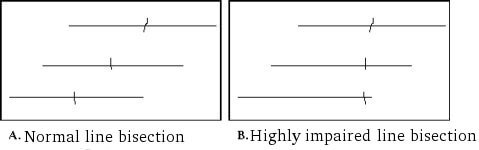
The Line Bisection Test is a test is a quick measure to detect the presence of unilateral spatial neglect (USN). To complete the test, one must place a mark with a pencil through the center of a series of horizontal lines. Usually, a displacement of the bisection mark towards the side of the brain lesion is interpreted as a symptom of neglect.
In-Depth Review
Purpose of the measure
The Line Bisection Test is a test is a quick measure to detect the presence of unilateral spatial neglect (USN). To complete the test, one must place a mark with a pencil through the center of a series of horizontal lines. Usually, a displacement of the bisection mark towards the side of the brain lesion is interpreted as a symptom of neglect.
Available versions
There are many versions of the Line Bisection Test, and the procedures are rarely standardized, with the exception of when the Line Bisection Test is used as an item within a standardized test battery (Plummer, Morris, & Dunai, 2003).
The relationship between abnormal line bisection and visual neglect has been observed for over a century (e.g. Axenfeld, 1894; Liepmann & Kalmus, 1900). In 1980, Schenkenberg, Bradford, and Ajax formally evaluated this method of detecting the presence of visual neglect in patients with lesions of the non-dominant hemisphere, and are thought to be the first to statistically evaluate this method.
Features of the measure
Items:
Patients are asked to place a mark with a pencil (with their preferred or unaffected hand) through the center of a series of 18 horizontal lines on an 11x 8.5-inch page.
Scoring:
The test is scored by measuring the deviation of the bisection from the true center of the line. A deviation of more than 6 mm from the midpoint indicates USN. Omission of two or more lines on one half of the page indicates USN.
Time:
The test takes less than 5 minutes to complete.
Training:
None typically reported.
Subscales:
None.
Equipment:
- 11x 8.5-inch page of paper with 18 horizontal lines
- Pencil
Alternative form of the Line Bisection Test
The Line Bisection Test can be presented in various forms. Some studies use 18 horizontal lines, while others have used a single line (Parton, Malhotra & Husain, 2004), or a series of 10 lines (Ferber & Karnath, 2001). The Line Bisection Test is also offered as part of some standardized test batteries such as within the Behavioural Inattention Test (Wilson, Cockburn, Halligan, 1987; Schubert & Spatt, 2001).
Client suitability
Can be used with:
- Patients with stroke
Also called a “brain attack” and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a “schemic stroke”, or the formation of a blood clot in a vessel supplying blood to the brain.. - Patients must be able to hold a pencil in order to complete the task (the presence of apraxia may impair this ability).
Should not be used with:
- The Line Bisection Test should be used with caution in the clinical diagnosis of spatial neglect:
Ferber and Karnath (2001) found that deviation in line bisection was not apparent in 40% of the patients in their sample that had severe neglect. In comparison, each of the four cancellation tests administered in this study (Line Crossing, Letter Cancellation, Star Cancellation Test and Bells Test) missed 6% of the subjects and may be preferred over the Line Bisection Test for diagnosing USN. - Performance on the Line Bisection Test may be influenced by or may be indicative of other syndromes besides spatial neglect, such as hemianopia (damage of optic pathways that result in loss of vision in half of the visual field) (Ferber & Karnath, 2001). Consequently, the Line Bisection Test is not a highly specific measure of USN.
In what languages is the measure available?
Not applicable.
Summary
| What does the tool measure? | Unilateral Spatial Neglect (USN) in the extrapersonal space |
| What types of clients can the tool be used for? | Patients with stroke |
| Is this a screening or assessment tool? |
Screening . |
| Time to administer | Less than 5 minutes. |
| Versions |
There are many versions of the Line Bisection Test, and the procedures are rarely standardized, with the exception of when the Line Bisection Test is used as an item within a standardized test battery such as in the Behavioural Inattention Test. |
| Other Languages | Not applicable. |
| Measurement Properties | |
| Reliability |
Test-retest: Four studies have examined the test-retest reliability of the Line Bisection Test. Three studies reported excellent test-retest and one study reported adequate test-retest. |
| Validity |
Criterion: One study reported that when the Line Bisection Test was compared to other cancellation tests, the sensitivity of the test for detecting visuo-spatial neglect in elderly patients with stroke Construct: |
| Does the tool detect change in patients? | Not applicable. |
| Acceptability | The Line Bisection Test should be used as a screening tool rather than for clinical diagnosis of USN. Performance on the Line Bisection Test may be influenced by or may be indicative of other syndromes besides spatial neglect, such as hemianopia. Apraxia must be ruled out as this may affect the validity of test results. This test cannot be completed by proxy. Patients must be able to hold a pencil to complete. |
| Feasibility | The Line Bisection Test takes only 5 minutes to complete and is simple to score. Only simple equipment is required (a pencil and paper with 18 horizontal lines). |
| How to obtain the tool? |
The Line Bisection Test can be purchased as part of the Behavioural Inattention Test from Pearson Assessment by clicking on the following link:http://pearsonassess.ca/haiweb/Cultures/en-CA/Products/Product+Detail.htm?CS_Category=&CS_Catalog=TPC-CACatalog&CS_ProductID=749129972 |
Psychometric Properties
Overview
For the purposes of this review, we conducted a literature search to identify all relevant publications on the psychometric properties of the Line Bisection Test. The test has been evaluated in many studies for its criterion validity
, resulting in evidence of its strong psychometric properties in comparison to other paper-and-pencil tests (Menon & Korner-Bitensky, 2004).
Reliability
Test-retest:
Schenkenberg et al. (1980) examined the test-retest reliability
of the Line Bisection Test in patients with right-hemisphere lesions, diffuse lesions, left-hemisphere lesions, and hospital controls, and found that it had excellent test-retest reliability
, ranging from r = 0.84 to r = 0.93.
Similarly, Chen-Sea and Henderson (1994) reported an excellent test-retest reliability
of r = 0.93 for the Line Bisection Test.
Kinsella, Packer, Ng, Olver, and Stark (1995) found adequate test-retest reliability
for the Line Bisection Test (Pearson r = 0.64).
Bailey, Riddoch and Crome (2004) examined the test-retest reliability
of the Line Bisection Test in elderly patients with stroke
Validity
Criterion:
Bailey, Riddoch, and Crome (2000) found that when the Line Bisection Test was compared to other cancellation tests, the sensitivitySensitivity refers to the probability that a diagnostic technique will detect a particular disease or condition when it does indeed exist in a patient (National Multiple Sclerosis Society). See also “Specificity.”
of the test for detecting visuo-spatial neglect in elderly patients with strokeAlso called a “brain attack” and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a “schemic stroke”, or the formation of a blood clot in a vessel supplying blood to the brain. was 76.4%.
Construct:
Marsh and Kersel (1993) examined the construct validityReflects the ability of an instrument to measure an abstract concept, or construct. For some attributes, no gold standard exists. In the absence of a gold standard , construct validation occurs, where theories about the attribute of interest are formed, and then the extent to which the measure under investigation provides results that are consistent with these theories are assessed.
of the Line Bisection Test by correlating the test with the Star Cancellation Test using Pearson’s correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases – for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases – for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
in a sample of 27 rehabilitation patients with a history of strokeAlso called a “brain attack” and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a “schemic stroke”, or the formation of a blood clot in a vessel supplying blood to the brain.. The two measures were found to have an adequate negative correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases – for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases – for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
(r = -0.40). The correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases – for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases – for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
is negative because a high score on the Line Bisection Test indicates USN, however a score close to 0 on the Star Cancellation Test indicates the absence of USN.
Egelko et al. (1988) correlated Line Bisection Test scores with mean CT-scan damage, and CT-scan damage of temporal lobe, parietal lobe, and occipital lobe. All correlations were found to be adequate (r = -0.44, -0.59,-0.37, and -0.42, respectively).
Friedman (1990) examined whether the Line Bisection Test correlated with functional outcome in 82 elderly patients within 14 days of a non-lacunar strokeAlso called a “brain attack” and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a “schemic stroke”, or the formation of a blood clot in a vessel supplying blood to the brain.. At discharge assessment, patients with impaired line bisection had poorer functional outcome than those with normal line bisection as measured by Barthel Index scores, walking speed and discharge destination. When subjects with impaired line bisection were divided into two groups according to line bisection score, the severely impaired had worse functional outcome than the mildly impaired.
Convergent:
Agrell, Dehlin, and Dahlgren (1997) compared the performance of 57 elderly patients with strokeAlso called a “brain attack” and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a “schemic stroke”, or the formation of a blood clot in a vessel supplying blood to the brain. on 5 different tests for visuo-spatial neglect (Star Cancellation Test, Line Crossing-Albert’s Test, Line Bisection, Clock Drawing Test and Copy A Cross). The Line Bisection Test had an excellent correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases – for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases – for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
with Line Crossing-Albert’s Test (r = 0.85) and correlated adequately with the Star Cancellation Test (r = -0.33).
Bailey, Riddoch, and Crome (2000) administered the Line Bisection Test and the Baking Tray Task to 107 patients with right or left sided brain damage and 43 age-matched controls. The Baking Tray Task had an excellent correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases – for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases – for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
with the Line Bisection Test (r = -0.66). This correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases – for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases – for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
is negative because a high score on the Line Bisection Test indicates the presence of USN, whereas a high score on the Baking Tray Task indicates normal performance.
Binder, Marshall, Lazer, Benjamin, and Mohr (1992) compared the performance on line bisection with that on Letter Cancellation in a group of 34 patients with right-sided brain damage. They found no significant correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases – for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases – for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
(r = 0.39) between the scores in the two tests.
Similarly, Schubert and Spatt (2001) found that in 20 patients with right hemisphere strokeAlso called a “brain attack” and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a “schemic stroke”, or the formation of a blood clot in a vessel supplying blood to the brain., no significant correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases – for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases – for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
between the Line Bisection Test and the Star Cancellation Test were found (r = 0.48). Furthermore, five patients with impaired performance on one of the tests were within the normal range on the other one.
Ishiai, Sugishita, Ichikawa, Gono, and Watabiki (1993) examined the construct validityReflects the ability of an instrument to measure an abstract concept, or construct. For some attributes, no gold standard exists. In the absence of a gold standard , construct validation occurs, where theories about the attribute of interest are formed, and then the extent to which the measure under investigation provides results that are consistent with these theories are assessed.
of the Clock Drawing Test and found that it had a poor correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases – for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases – for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
with the Line Bisection Test (r = 0.05).
Known groups:
Schenkenberg et al. (1980) reported that Line Bisection Test performance can discriminate between patients with right-hemisphere lesions and patients with diffuse lesions, patients with left-hemisphere lesions, and hospital controls.
Responsiveness
No evidence.
References
- Agrell, B. M., Dehlin, O. I., Dahlgren, C. J. (1997). Neglect in elderly stroke patients: a comparison of five tests. Psychiatry Clin Neurosci, 51(5), 295-300.
- Axenfeld, D. (1894). Eine einfache Methode Hemianopsie zu constatiren. Neurol Centralbl, 437-438.
- Bailey, M. J., Riddoch, M. J., Crome, P. (2000). Evaluation of a test battery for hemineglect in elderly stroke patients for use by therapists in clinical practice. NeuroRehabilitation, 14, 139-150.
- Bailey, M. J., Riddoch, M. J., Crome, P. (2004). Test-retest stability of three tests for unilateral visual neglect in patients with stroke: Star Cancellation, Line Bisection, and the Baking Tray Task. Neurophsychological Rehabilitation, 14(4), 403-419.
- Barton, J. J. S., Black, S. E. (1998). Line bisection in hemianopia. J Neurol Neurosurg Psychiatry, 64, 660-662.
- Binder, J., Marshall, R., Lazar, R., Benjamin, J., Mohr, J. P. (1992). Distinct syndromes of hemineglect. Archiv Neurology, 49, 1187-1194.
- Chen-Sea, M. J., Henderson, A. (1994). The reliability and validity of visuospatial inattention tests with stroke patients. Occup Ther Int, 1, 36-48.
- Egelko, S., Gordon, W. A., Hibbard, M. R., Diller, L., Lieberman, A., Holliday, R., Ragnarsson, K., Shaver, M. S., Orazem, J. (1988). Relationship among CT scans, neurological exam, and neuropsychological test performance in right-brain-damaged stroke patients. J Clin Exp Neuropsychol, 10, 539-564.
- Ferber, S., Karnath, H. O. (2001). How to assess spatial neglect–Line Bisection or Cancellation Tests? J Clin Expl Neuropsychol, 23, 599-607.
- Friedman, P. J. (1990). Spatial neglect in acute stroke: the Line Bisection Test. Scand J Rehabil Med, 22, 101-106.
- Ishiai,S., Sugishita, M., Ichikawa, T., Gono, S., Watabiki, S. (1993). Clock-drawing test and unilateral spatial neglect. Neurology. 43, 106-110.
- Kinsella, G., Packer, S., Ng, K., Olver, J., Stark, R. (1995). Continuing issues in the assessment of neglect. Neuropsychological Rehabilitation, 5(3), 239-258.
- Liepmann, H., Kalmus, E. (1900). Ãœber einer Augenma beta störung beu Hemianopikern. Berlin Klin Wochenschr, 38, 838-842.
- Marsh, N. V., Kersel, D. A. (1993). Screening tests for visual neglect following stroke. Neuropsychological Rehabilitation, 3, 245-257.
- Menon, A., Korner-Bitensky, N. (2004). Evaluating unilateral spatial neglect post stroke: Working your way through the maze of assessment choices. Topics in Stroke Rehabilitation, 11(3), 41-66.
- Parton, A., Malhotra, P., Husain, M. (2004). Hemispatial neglect. J Neurol Neurosurg Psychiatry, 75, 13-21.
- Plummer, P., Morris, M. E., Dunai, J. (2003). Assessment of unilateral neglect. Phys Ther, 83(8), 732-740.
- Schenkenberg, T., Bradford, D. C., Ajax, E. T. (1980). Line bisection and unilateral visual neglect in patients with neurological impairment. Neurology. 30, 509-517.
- Schubert, F., Spatt, J. (2001). Double dissociations between neglect tests: Possible relation to lesion site. Eur Neurol, 45, 160-164.
- Wilson, B. A., Cockburn, J., Halligan, P. W. (1987). Behavioural Inattention Test. Titchfield, Hants, England: Thames Valley Test Company Ltd.
See the measure
How to obtain the Line Bisection Test?
Click here to obtain a copy of the Line Bisection Test
The Line Bisection Test can be purchased as part of the Behavioural Inattention Test from Pearson Assessment by clicking on the following link: Pearson Assessment