Purpose
The Timed Up and Go (TUG) is a screening tool used to test basic mobility skills of frail elderly patients (60-90 years old). The TUG can be used with, but is not limited to, persons with stroke.
In-Depth Review
Purpose of the measure
The TUG is a general physical performance test used to assess mobility, balance and locomotor performance in elderly people with balance disturbances. More specifically, it assesses the ability to perform sequential motor tasks relative to walking and turning (Schoppen, Boonstra, Groothoff, de Vries, Goeken, & Eisma, 1999; Morris, Morris, & Iansek, 2001).
Available versions
The “Get Up and Go” test (the original TUG) was developed by Mathias, Nayak, and Issacs in 1986.
The TUG was published by Podsiadlo and Richardson in 1991 to address the issues of poor inter-rater reliabilityA method of measuring reliability . Inter-rater reliability determines the extent to which two or more raters obtain the same result when using the same instrument to measure a concept.
observed with intermediate scores in the “Get Up and Go”. The TUG incorporates time as the measuring component to assess general balance and function.
Features of the measure
Items:
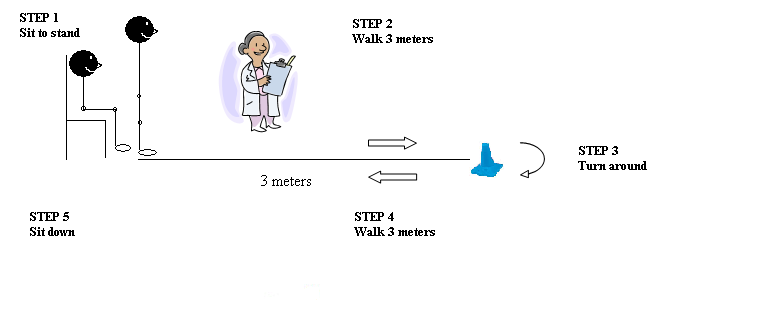
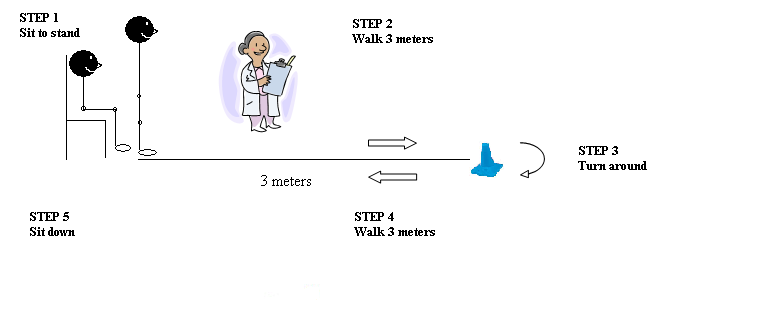
There are no actual items in the TUG. The individual must stand up from a chair (which should not be leaned up against a wall), walk a distance of 3 meters, turn around, walk back to the chair and sit down – all performed at a comfortable and safe pace (Figure 1). One practice trial is permitted to allow the individual to familiarize him/herself with the task. Timing commences with the verbal instruction “go” and stops when the client returns to seated position. The individual wears their regular footwear and is permitted to use their walking aid (cane/walker) with its use indicated on the data collection form. No physical assistance is given.
Figure 1.
Scoring:
Performance of the TUG is rated on a scale from 1 to 5 where 1 indicates “normal function” and 5 indicates “severely abnormal function” according to the observer’s perception of the individual’s risk of falling (Podsiadlo & Richardson, 1991). The score consists of the time taken to complete the test activity, in seconds.
Steffen, Hacker and Mollinger (2002) reported that on average, healthy individuals between the ages of 60-80 years complete the TUG in 10 seconds or less. Males between the ages of 80-89 years old take on average 10 ± 1 seconds to complete, and women take 11 ± 3 seconds to complete. Formal norms have not yet been established for patients with strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain..
Standardized cut-off scores to predict risk of falling have not yet been established. In one study, a cut-off score of ? 13.5 seconds has been shown to predict falling in community-dwelling frail elders, but this score has not been verified in other studies (Shumway-Cook et al., 2000).
Scoring and interpretation of the TUG
| Score |
Interpretation |
| < 10s |
Completely independent
With or without walking aid for ambulation and transfers |
| < 20s |
Independent for main transfers
With or without walking aid, independent for basic tub or shower transfers and able to climb most stairs and go outside alone |
| > 30s |
Requires assistance
Dependent in most activitiesAs defined by the International Classification of Functioning, Disability and Health, activity is the performance of a task or action by an individual. Activity limitations are difficulties in performance of activities. These are also referred to as function.
|
(Adapted from Podsiadlo & Richardson, 1991)
Subscales:
None typically reported.
Equipment:
The TUG does not require any specialized equipment and can therefore be accomplished in community as well as institutional settings.
- Standard chair with armrests (46cm seat height and 63-65cm armrest height)
- Tape measure
- Brightly colored tape or cone to mark off the 3m path 3m path free from obstruction
- Stopwatch or wrist watch with a second hand to time the performance.
Training:
Minimal training is required to score the test or interpret the results. The assessor should be aware of safety issues during mobility in individuals with strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain..
Time:
The TUG requires 1 to 2 minutes to administer (Finch, Brooks, Stratford, & Mayo, 2002).
Alternative forms of the TUG
- TUG Cognitive (Shumway-Cook, Brauer, & Woollacott, 2000). In the TUG Cognitive, patients must complete the task while counting backwards from a randomly selected number between 20 and 100.
- TUG Manual (Lundin-Olsson et al., 1998). In the TUG Manual, patients must complete the task while carrying a full cup of water. Lundin-Olsson et al. (1998) found that frail older adults who had a time difference of greater than 4.5 seconds between the TUG Manual and the TUG were more prone to falls during the following 6 months.
Client suitability
Can be used with:
Patients with strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain.
- The TUG can be administered to geriatric clients ? 65 years old with any diagnosis (e.g. arthritis, strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain., vertigo, Parkinson’s disease, cerebellar disorders and general deconditioning) (Shumway-Cook & Woollacott, 2001; Hayes & Johnson, 2003; Morris et al., 2001).
- The TUG can also be used with patients ? 18 years old with an acute neurological diagnosis (Shumway-Cook & Woollacott, 2001).
- Clients must be able to walk approximately 6 meters with or without an assistive device but without the assistance of another person.
- Clients must have sufficient vision to walk to the 3-meter line.
- Non-English speakers must receive appropriate translation.
Should not be used in:
- The TUG is not appropriate for clients with severe cognitive impairments that prevent understanding of the tasks. Rockwood, Awalt, Carver, and MacKnight (2000) found that in cognitively impaired frail elderly individuals, 35.5% were unable to physically perform the test.
- Severely affected patients such as those who cannot leave a seated position. There may be a floor effectThe floor effect is when data cannot take on a value lower than some particular number. Thus, it represents a subsample for whom clinical decline may not register as a change in score, even if there is worsening of function/behavior etc. because there are no items or scaling within the test that measure decline from the lowest possible score. See also "ceiling effect."
with these patients. Instead, you may wish to consider the Postural Assessment Scale for StrokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. Patients (PASS), which was designed as a balance assessment for patients with strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. and is applicable for all patients with strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain., even those with the most severe postural performance (Benaim, Pérennou, Villy, Rousseaux, & Pelissier, 1999).
- Since the TUG is administered through direct observation of task completion. A proxy respondent cannot complete it.
- The TUG is a limited measure assessing few aspects of balance. For a more comprehensive measure of balance, the Postural Assessment Scale for StrokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. Patients (PASS) (Benaim et al., 1999) or the Berg Balance Scale (Berg, Wood-Dauphinee, Williams, & Maki, 1992) is suggested.
In what languages is the measure available?
Given the simplicity of the instructions, the TUG can be administered in different languages with informal translations (Tremblay, Savard, Casimiro, & Tremblay, 2004).
Summary
| What does the tool measure? |
Basic mobility and balance in frail elderly patients |
| What types of clients can the tool be used for? |
Elderly patients (60-90 years old), patients with strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. |
Is this a screeningTesting for disease in people without symptoms.
or assessment tool? |
ScreeningTesting for disease in people without symptoms.
|
| Time to administer |
1-2 minutes |
| Versions |
TUG Cognitive, TUG Manual |
| Other Languages |
Can be completed in any language |
| Measurement Properties |
ReliabilityReliability can be defined in a variety of ways. It is generally understood to be the extent to which a measure is stable or consistent and produces similar results when administered repeatedly. A more technical definition of reliability is that it is the proportion of "true" variation in scores derived from a particular measure. The total variation in any given score may be thought of as consisting of true variation (the variation of interest) and error variation (which includes random error as well as systematic error). True variation is that variation which actually reflects differences in the construct under study, e.g., the actual severity of neurological impairment. Random error refers to "noise" in the scores due to chance factors, e.g., a loud noise distracts a patient thus affecting his performance, which, in turn, affects the score. Systematic error refers to bias that influences scores in a specific direction in a fairly consistent way, e.g., one neurologist in a group tends to rate all patients as being more disabled than do other neurologists in the group. There are many variations on the measurement of reliability including alternate-forms, internal consistency , inter-rater agreement , intra-rater agreement , and test-retest .
|
Internal consistencyA method of measuring reliability . Internal consistency reflects the extent to which items of a test measure various aspects of the same characteristic and nothing else. Internal consistency coefficients can take on values from 0 to 1. Higher values represent higher levels of internal consistency.:
No studies have examined the internal consistencyA method of measuring reliability . Internal consistency reflects the extent to which items of a test measure various aspects of the same characteristic and nothing else. Internal consistency coefficients can take on values from 0 to 1. Higher values represent higher levels of internal consistency. of the TUG.
Test-retest:
Out of seven studies examining the test-retest reliabilityA way of estimating the reliability of a scale in which individuals are administered the same scale on two different occasions and then the two scores are assessed for consistency. This method of evaluating reliability is appropriate only if the phenomenon that the scale measures is known to be stable over the interval between assessments. If the phenomenon being measured fluctuates substantially over time, then the test-retest paradigm may significantly underestimate reliability. In using test-retest reliability, the investigator needs to take into account the possibility of practice effects, which can artificially inflate the estimate of reliability (National Multiple Sclerosis Society).
of the TUG.
Intra-rater:
Out of two studies examining the intra-rater reliabilityThis is a type of reliability assessment in which the same assessment is completed by the same rater on two or more occasions. These different ratings are then compared, generally by means of correlation. Since the same individual is completing both assessments, the rater's subsequent ratings are contaminated by knowledge of earlier ratings.
of the TUG.
Inter-rater:
Out of five studies examining the inter-rater reliabilityA method of measuring reliability . Inter-rater reliability determines the extent to which two or more raters obtain the same result when using the same instrument to measure a concept.
of the TUG, and one reported no significant difference in scoring between two raters, suggesting high inter-rater reliabilityA method of measuring reliability . Inter-rater reliability determines the extent to which two or more raters obtain the same result when using the same instrument to measure a concept.
. |
ValidityThe degree to which an assessment measures what it is supposed to measure.
|
Content:
Not available.
Criterion:
No gold standardA measurement that is widely accepted as being the best available to measure a construct.
exists.
Predictive:
TUG has been found to predict nursing home placement and risk of falling.
Construct:
Excellent correlations between the TUG and the Older Americans Resources and Services Instrumental ActivitiesAs defined by the International Classification of Functioning, Disability and Health, activity is the performance of a task or action by an individual. Activity limitations are difficulties in performance of activities. These are also referred to as function.
of Daily Living Scale (OARS IADL), OARS ActivitiesAs defined by the International Classification of Functioning, Disability and Health, activity is the performance of a task or action by an individual. Activity limitations are difficulties in performance of activities. These are also referred to as function.
of Daily Living (OARS ADL), Frailty Scale, Berg Balance Scale, Tinetti Balance Scale, measures of gaitThe pattern of walking, which is often characterized by elements of progression, efficiency, stability and safety.
speed (one study reported adequate correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases - for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases - for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
), and 6-Minute Walk Test (6MWT). Adequate correlations with the Barthel Index, Functional Independence Measure, Groningen Activity Restriction Scale, Sickness Impact Profile.
Known groups:
The TUG can distinguish between elderly patients using different ambulatory aids, the presence of cognitive impairment, patients with Parkinson’s disease who were on the medication levodopa and those patients who were not on levodopa, and healthy elderly individuals from patients with strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain.. |
| Does the tool detect change in patients? |
In one study, 35.5% of frail elderly individuals with cognitive impairment were unable to physically perform the test, which may be indicative of a large floor effectThe floor effect is when data cannot take on a value lower than some particular number. Thus, it represents a subsample for whom clinical decline may not register as a change in score, even if there is worsening of function/behavior etc. because there are no items or scaling within the test that measure decline from the lowest possible score. See also "ceiling effect."
.
Although the TUG has been developed as a screeningTesting for disease in people without symptoms.
ability to detect change. Another study reported that out of a number of gaitThe pattern of walking, which is often characterized by elements of progression, efficiency, stability and safety.
speed measures, the TUG was the most able to detect change.
|
| Acceptability |
TUG is a short and simple measure that takes only a few minutes to complete and requires only a few basic movements. The TUG has been found to have less reliabilityReliability can be defined in a variety of ways. It is generally understood to be the extent to which a measure is stable or consistent and produces similar results when administered repeatedly. A more technical definition of reliability is that it is the proportion of "true" variation in scores derived from a particular measure. The total variation in any given score may be thought of as consisting of true variation (the variation of interest) and error variation (which includes random error as well as systematic error). True variation is that variation which actually reflects differences in the construct under study, e.g., the actual severity of neurological impairment. Random error refers to "noise" in the scores due to chance factors, e.g., a loud noise distracts a patient thus affecting his performance, which, in turn, affects the score. Systematic error refers to bias that influences scores in a specific direction in a fairly consistent way, e.g., one neurologist in a group tends to rate all patients as being more disabled than do other neurologists in the group. There are many variations on the measurement of reliability including alternate-forms, internal consistency , inter-rater agreement , intra-rater agreement , and test-retest .
among patients with cognitive impairment. |
| Feasibility |
TUG requires no specialized equipment. Although only minimal training is required, the assessor must be aware of safety issues during mobility in individuals with strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain.. |
| How to obtain the tool? |
The TUG can be obtained by contacting the developer, Diane Podsiadlo, CLSC NDG, 2525 Boulevard Cavendish, Bureau 110, Montreal, QC, H4B 2Y4. Fax: 514-485-6406 |
Psychometric Properties
Overview
There is a paucity of literature published on the reliabilityReliability can be defined in a variety of ways. It is generally understood to be the extent to which a measure is stable or consistent and produces similar results when administered repeatedly. A more technical definition of reliability is that it is the proportion of "true" variation in scores derived from a particular measure. The total variation in any given score may be thought of as consisting of true variation (the variation of interest) and error variation (which includes random error as well as systematic error). True variation is that variation which actually reflects differences in the construct under study, e.g., the actual severity of neurological impairment. Random error refers to "noise" in the scores due to chance factors, e.g., a loud noise distracts a patient thus affecting his performance, which, in turn, affects the score. Systematic error refers to bias that influences scores in a specific direction in a fairly consistent way, e.g., one neurologist in a group tends to rate all patients as being more disabled than do other neurologists in the group. There are many variations on the measurement of reliability including alternate-forms, internal consistency , inter-rater agreement , intra-rater agreement , and test-retest .
and validityThe degree to which an assessment measures what it is supposed to measure.
of the TUG in patients with strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain.. For the purposes of this review, we conducted a literature search to identify all relevant publications on the psychometric properties of the TUG.
Floor and Ceiling Effects
Rockwood et al. (2000) found that in frail elderly individuals with cognitive impairment, 35.5% were unable to physically perform the test. This may be indicative of the presence of a large floor effectThe floor effect is when data cannot take on a value lower than some particular number. Thus, it represents a subsample for whom clinical decline may not register as a change in score, even if there is worsening of function/behavior etc. because there are no items or scaling within the test that measure decline from the lowest possible score. See also "ceiling effect."
with the TUG.
Reliability
Internal consistencyA method of measuring reliability . Internal consistency reflects the extent to which items of a test measure various aspects of the same characteristic and nothing else. Internal consistency coefficients can take on values from 0 to 1. Higher values represent higher levels of internal consistency.:
Not reported
Test-retest:
Podsiadlo and Richardson (1991) reported excellent test-retest reliabilityA way of estimating the reliability of a scale in which individuals are administered the same scale on two different occasions and then the two scores are assessed for consistency. This method of evaluating reliability is appropriate only if the phenomenon that the scale measures is known to be stable over the interval between assessments. If the phenomenon being measured fluctuates substantially over time, then the test-retest paradigm may significantly underestimate reliability. In using test-retest reliability, the investigator needs to take into account the possibility of practice effects, which can artificially inflate the estimate of reliability (National Multiple Sclerosis Society).
of the TUG in frail elderly patients (ICC = 0.99).
Steffen et al. (2002) administered the TUG to 97 community-dwelling older adults. The test-retest reliabilityA way of estimating the reliability of a scale in which individuals are administered the same scale on two different occasions and then the two scores are assessed for consistency. This method of evaluating reliability is appropriate only if the phenomenon that the scale measures is known to be stable over the interval between assessments. If the phenomenon being measured fluctuates substantially over time, then the test-retest paradigm may significantly underestimate reliability. In using test-retest reliability, the investigator needs to take into account the possibility of practice effects, which can artificially inflate the estimate of reliability (National Multiple Sclerosis Society).
of the TUG was found to be excellent in this population (ICC = 0.97).
Thompson and Medley (1995) examined the test-retest reliabilityA way of estimating the reliability of a scale in which individuals are administered the same scale on two different occasions and then the two scores are assessed for consistency. This method of evaluating reliability is appropriate only if the phenomenon that the scale measures is known to be stable over the interval between assessments. If the phenomenon being measured fluctuates substantially over time, then the test-retest paradigm may significantly underestimate reliability. In using test-retest reliability, the investigator needs to take into account the possibility of practice effects, which can artificially inflate the estimate of reliability (National Multiple Sclerosis Society).
of the TUG in elderly individuals without any health problems and found excellent test-retest correlations ranging from 0.81 to 0.99.
Rockwood et al. (2000) examined the test-retest reliabilityA way of estimating the reliability of a scale in which individuals are administered the same scale on two different occasions and then the two scores are assessed for consistency. This method of evaluating reliability is appropriate only if the phenomenon that the scale measures is known to be stable over the interval between assessments. If the phenomenon being measured fluctuates substantially over time, then the test-retest paradigm may significantly underestimate reliability. In using test-retest reliability, the investigator needs to take into account the possibility of practice effects, which can artificially inflate the estimate of reliability (National Multiple Sclerosis Society).
of the TUG as part of the Canadian Study of Health and Aging. Adequate test-retest reliabilityA way of estimating the reliability of a scale in which individuals are administered the same scale on two different occasions and then the two scores are assessed for consistency. This method of evaluating reliability is appropriate only if the phenomenon that the scale measures is known to be stable over the interval between assessments. If the phenomenon being measured fluctuates substantially over time, then the test-retest paradigm may significantly underestimate reliability. In using test-retest reliability, the investigator needs to take into account the possibility of practice effects, which can artificially inflate the estimate of reliability (National Multiple Sclerosis Society).
was reported for all participants (ICC = 0.56), for individuals without cognitive impairment alone (ICC = 0.50), and for those with cognitive impairment alone (ICC = 0.56). The results of this study are substantially lower than the results of previous studies examining the test-retest reliabilityA way of estimating the reliability of a scale in which individuals are administered the same scale on two different occasions and then the two scores are assessed for consistency. This method of evaluating reliability is appropriate only if the phenomenon that the scale measures is known to be stable over the interval between assessments. If the phenomenon being measured fluctuates substantially over time, then the test-retest paradigm may significantly underestimate reliability. In using test-retest reliability, the investigator needs to take into account the possibility of practice effects, which can artificially inflate the estimate of reliability (National Multiple Sclerosis Society).
of the TUG in elderly patients. The authors suggest this may be due to the fact that unlike other similar studies, they did not exclude medically unstable patients in their study, and further, they did not control for certain factors (e.g. the time and setting in which the TUG was readministered).
Morris et al. (2001) examined the test-retest reliabilityA way of estimating the reliability of a scale in which individuals are administered the same scale on two different occasions and then the two scores are assessed for consistency. This method of evaluating reliability is appropriate only if the phenomenon that the scale measures is known to be stable over the interval between assessments. If the phenomenon being measured fluctuates substantially over time, then the test-retest paradigm may significantly underestimate reliability. In using test-retest reliability, the investigator needs to take into account the possibility of practice effects, which can artificially inflate the estimate of reliability (National Multiple Sclerosis Society).
of the TUG in 12 patients with Parkinson’s disease and 12 subjects without Parkinson’s disease. Patients were videotaped and timed by 2 experienced raters. Three experienced clinicians and 3 inexperienced clinicians later rated the videotape. The test-retest reliabilityA way of estimating the reliability of a scale in which individuals are administered the same scale on two different occasions and then the two scores are assessed for consistency. This method of evaluating reliability is appropriate only if the phenomenon that the scale measures is known to be stable over the interval between assessments. If the phenomenon being measured fluctuates substantially over time, then the test-retest paradigm may significantly underestimate reliability. In using test-retest reliability, the investigator needs to take into account the possibility of practice effects, which can artificially inflate the estimate of reliability (National Multiple Sclerosis Society).
of the TUG was found to be excellent (ranging from r = 0.87 to r = 0.99).
Flansbjer, Holmback, Downham, Patten, and Lexell (2005) assessed the test-retest reliabilityA way of estimating the reliability of a scale in which individuals are administered the same scale on two different occasions and then the two scores are assessed for consistency. This method of evaluating reliability is appropriate only if the phenomenon that the scale measures is known to be stable over the interval between assessments. If the phenomenon being measured fluctuates substantially over time, then the test-retest paradigm may significantly underestimate reliability. In using test-retest reliability, the investigator needs to take into account the possibility of practice effects, which can artificially inflate the estimate of reliability (National Multiple Sclerosis Society).
of the TUG in 50 patients with chronic mild to moderate post-stroke hemiparesis. The patients performed the TUG twice, with 7 days between each evaluation. The test-retest reliabilityA way of estimating the reliability of a scale in which individuals are administered the same scale on two different occasions and then the two scores are assessed for consistency. This method of evaluating reliability is appropriate only if the phenomenon that the scale measures is known to be stable over the interval between assessments. If the phenomenon being measured fluctuates substantially over time, then the test-retest paradigm may significantly underestimate reliability. In using test-retest reliability, the investigator needs to take into account the possibility of practice effects, which can artificially inflate the estimate of reliability (National Multiple Sclerosis Society).
of the TUG was found to be excellent (ICC = 0.96).
Ng and Hui-Chan (2005) administered the TUG to 10 healthy elderly subjects and 10 patients with chronic strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. twice, at the same time of day, on different days within one week. The results showed excellent test-retest reliabilityA way of estimating the reliability of a scale in which individuals are administered the same scale on two different occasions and then the two scores are assessed for consistency. This method of evaluating reliability is appropriate only if the phenomenon that the scale measures is known to be stable over the interval between assessments. If the phenomenon being measured fluctuates substantially over time, then the test-retest paradigm may significantly underestimate reliability. In using test-retest reliability, the investigator needs to take into account the possibility of practice effects, which can artificially inflate the estimate of reliability (National Multiple Sclerosis Society).
for both healthy elderly subjects (ICC = 0.97) and patients with strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. (ICC = 0.95). The results of this study and the previous study by Flansbjer et al. (2005) suggest that the TUG is a reliable measure in patients with strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain..
Intra-rater:
Podsiadlo and Richardson (1991) found that the TUG demonstrated excellent intra-rater reliabilityThis is a type of reliability assessment in which the same assessment is completed by the same rater on two or more occasions. These different ratings are then compared, generally by means of correlation. Since the same individual is completing both assessments, the rater's subsequent ratings are contaminated by knowledge of earlier ratings.
in frail elderly individuals (ICC= 0.99).
Schoppen et al. (1999) examined the intra-rater reliabilityThis is a type of reliability assessment in which the same assessment is completed by the same rater on two or more occasions. These different ratings are then compared, generally by means of correlation. Since the same individual is completing both assessments, the rater's subsequent ratings are contaminated by knowledge of earlier ratings.
of the TUG in elderly patients with a lower-extremity amputation. Patients performed the TUG for one observer at two different occasions with an interval of two weeks. An excellent Spearman correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases - for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases - for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
was observed between scores obtained by the same rater on two consecutive visits (r = 0.93).
Note: Caution should be taken in interpreting these findings as the Spearman correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases - for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases - for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
is not the preferred method of assessing intra-rater reliabilityThis is a type of reliability assessment in which the same assessment is completed by the same rater on two or more occasions. These different ratings are then compared, generally by means of correlation. Since the same individual is completing both assessments, the rater's subsequent ratings are contaminated by knowledge of earlier ratings.
and may have produced higher reliabilityReliability can be defined in a variety of ways. It is generally understood to be the extent to which a measure is stable or consistent and produces similar results when administered repeatedly. A more technical definition of reliability is that it is the proportion of "true" variation in scores derived from a particular measure. The total variation in any given score may be thought of as consisting of true variation (the variation of interest) and error variation (which includes random error as well as systematic error). True variation is that variation which actually reflects differences in the construct under study, e.g., the actual severity of neurological impairment. Random error refers to "noise" in the scores due to chance factors, e.g., a loud noise distracts a patient thus affecting his performance, which, in turn, affects the score. Systematic error refers to bias that influences scores in a specific direction in a fairly consistent way, e.g., one neurologist in a group tends to rate all patients as being more disabled than do other neurologists in the group. There are many variations on the measurement of reliability including alternate-forms, internal consistency , inter-rater agreement , intra-rater agreement , and test-retest .
coefficients than a more appropriate analysis.
Inter-rater:
Podsiadlo and Richardson (1991) compared the inter-rater reliabilityA method of measuring reliability . Inter-rater reliability determines the extent to which two or more raters obtain the same result when using the same instrument to measure a concept.
of the TUG, the TUG Manual and the TUG Cognitive using same day comparisons of three raters. Excellent inter-rater reliabilities were found for the TUG (ICC = 0.98), the TUG Manual (ICC = 0.99), and the TUG Cognitive (ICC = 0.99).
Siggeirsdottir, Jonsson, Jonsson, and Iwarsson (2002) examined the inter-rater reliabilityA method of measuring reliability . Inter-rater reliability determines the extent to which two or more raters obtain the same result when using the same instrument to measure a concept.
of the TUG in 31 elderly individuals in a retirement home. No significant difference was found between the two raters (mean difference = 0.04s). The results of this study suggest that the TUG has high inter-rater reliabilityA method of measuring reliability . Inter-rater reliability determines the extent to which two or more raters obtain the same result when using the same instrument to measure a concept.
.
Norén, Bogren, Bolin, and Stenstrom (2001) examined the inter-rater reliabilityA method of measuring reliability . Inter-rater reliability determines the extent to which two or more raters obtain the same result when using the same instrument to measure a concept.
of the TUG in patients with peripheral arthritis. The inter-rater reliabilityA method of measuring reliability . Inter-rater reliability determines the extent to which two or more raters obtain the same result when using the same instrument to measure a concept.
among three physiotherapists was found to be excellent (ICC = 0.97).
Schoppen et al. (1999) examined the inter-rater reliabilityA method of measuring reliability . Inter-rater reliability determines the extent to which two or more raters obtain the same result when using the same instrument to measure a concept.
of the TUG in elderly patients with a lower-extremity amputation. The test was performed for two different observers at different times of the same day. An excellent Spearman correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases - for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases - for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
was found between the scores of the two observers (r = 0.96), demonstrating the excellent inter-rater reliabilityA method of measuring reliability . Inter-rater reliability determines the extent to which two or more raters obtain the same result when using the same instrument to measure a concept.
of the TUG.
Note: Caution should be taken in interpreting these findings as the Spearman correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases - for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases - for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
is not the preferred method of assessing inter-rater reliabilityA method of measuring reliability . Inter-rater reliability determines the extent to which two or more raters obtain the same result when using the same instrument to measure a concept.
and may have produced higher reliabilityReliability can be defined in a variety of ways. It is generally understood to be the extent to which a measure is stable or consistent and produces similar results when administered repeatedly. A more technical definition of reliability is that it is the proportion of "true" variation in scores derived from a particular measure. The total variation in any given score may be thought of as consisting of true variation (the variation of interest) and error variation (which includes random error as well as systematic error). True variation is that variation which actually reflects differences in the construct under study, e.g., the actual severity of neurological impairment. Random error refers to "noise" in the scores due to chance factors, e.g., a loud noise distracts a patient thus affecting his performance, which, in turn, affects the score. Systematic error refers to bias that influences scores in a specific direction in a fairly consistent way, e.g., one neurologist in a group tends to rate all patients as being more disabled than do other neurologists in the group. There are many variations on the measurement of reliability including alternate-forms, internal consistency , inter-rater agreement , intra-rater agreement , and test-retest .
coefficients than a more appropriate analysis.
Morris et al. (2001) examined the inter-rater reliabilityA method of measuring reliability . Inter-rater reliability determines the extent to which two or more raters obtain the same result when using the same instrument to measure a concept.
of the TUG using three experienced raters and three inexperienced raters. Each rater viewed the sequence of performances for 12 patients with Parkinson’s disease and 12 comparison patients from videotape. Raters viewed the videotapes independently at least one week after testing. ICCs were excellent for both experienced and inexperienced raters, ranging from r = 0.87 to r = 0.99. The results of this study demonstrate the excellent inter-rater reliabilityA method of measuring reliability . Inter-rater reliability determines the extent to which two or more raters obtain the same result when using the same instrument to measure a concept.
of the TUG in patients with Parkinson’s disease.
Validity
Content:
Not available.
Criterion:
No gold standardA measurement that is widely accepted as being the best available to measure a construct.
exists.
Predictive:
Nikolaus, Bach, Oster, and Schlierf (1996) examined predictors of death, nursing home placement and hospital admission in 135 patients admitted to a geriatric hospital and discharged home. In a logistic regression analysis, baseline TUG scores were found to be an independent predictor for nursing home placement.
Schwartz et al. (1999) found that in a sample of elderly Mexican-American women, those with the best and worst performance on the TUG were more likely to fall than those with moderate performance.
Whitney, Marchetti, Schade, and Wrisley (2004) found that patients with vestibular disorders and a history of falls who scored > 11.1 seconds on the TUG were five times more likely to have reported a fall in the previous 6 months.
Construct:
Convergent/Discriminant:
Rockwood et al. (2000) examined the convergent and discriminant validityMeasures that should not be related are not. Discriminant validity examines the extent to which a measure correlates with measures of attributes that are different from the attribute the measure is intended to assess.
of the TUG using Phase 2 data from the Canadian Study of Health and Ageing. Both discriminant validityMeasures that should not be related are not. Discriminant validity examines the extent to which a measure correlates with measures of attributes that are different from the attribute the measure is intended to assess.
was assessed by comparing the TUG to other functional assessments including: the Older Americans Resources and Services Instrumental ActivitiesAs defined by the International Classification of Functioning, Disability and Health, activity is the performance of a task or action by an individual. Activity limitations are difficulties in performance of activities. These are also referred to as function.
of Daily Living Scale (OARS IADL) and OARS ActivitiesAs defined by the International Classification of Functioning, Disability and Health, activity is the performance of a task or action by an individual. Activity limitations are difficulties in performance of activities. These are also referred to as function.
of Daily Living (OARS ADL) (Fillenbaum & Smyer, 1981), the Cumulative Illness Rating Scale (CIRS) (Linn, Linn, & Gurel, 1968), and the Frailty Scale (developed for the Canadian Study of Health and Aging-2) using Spearman correlations. The TUG demonstrated excellent correlations with the OARS ADL for all participants, and with participants with cognitive impairment alone (r = -0.69 and r = -0.72 respectively). The OARS IADL also had excellent correlations with the TUG for all participants and with participants with cognitive impairment alone (r = -0.70 and r = -0.70, respectively). The TUG also had an excellent correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases - for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases - for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
with the Frailty Scale for all participants (r = 0.60). Some correlations are negative because a high score on the TUG indicates abnormal functioning, whereas a high score on some other measures indicates better performance. The TUG correlated poorly with the CIRS (ranging from r = 0.22 to 0.26).
Berg, Maki, Williams, Holliday, and Wood-Dauphinee (1992) compared scores from clinical measures and laboratory tests of balance and mobility in 31 elderly subjects. An adequate correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases - for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases - for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
between the TUG and the Barthel Index was reported (r = -0.48). Excellent correlations between the TUG and the Berg Balance Scale (r = -0.76) and between the TUG and the Tinetti Balance Scale (Tinetti, 1986) (r = 0.74) were also observed (some correlations are negative because a high score on the TUG abnormal functioning, whereas a high score on other measures indicates better health).
Podsiadlo and Richardson (1989) examined the convergent validityA type of validity that is determined by hypothesizing and examining the overlap between two or more tests that presumably measure the same construct. In other words, convergent validity is used to evaluate the degree to which two or more measures that theoretically should be related to each other are, in fact, observed to be related to each other.
of the TUG in frail elderly individuals and reported an excellent correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases - for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases - for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
between the TUG and the Berg Balance Scale (r = -0.72), and an adequate correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases - for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases - for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
between the TUG and gaitThe pattern of walking, which is often characterized by elements of progression, efficiency, stability and safety.
speed (r = -0.55) and between the TUG and the Barthel Index (r = -0.51).
Brooks, Davis, and Naglie (2006) examined the construct validityReflects the ability of an instrument to measure an abstract concept, or construct. For some attributes, no gold standard exists. In the absence of a gold standard , construct validation occurs, where theories about the attribute of interest are formed, and then the extent to which the measure under investigation provides results that are consistent with these theories are assessed.
of the TUG, and two other measures of physical performance in 52 frail older individuals. Correlations between the TUG and the Functional Independence Measure (Keith, Granger, Hamilton, & Sherwin, 1987) were adequate at both admission (r = -0.59) and at discharge (r = -0.42). Correlations are negative because a high score on the TUG indicates abnormal functioning whereas a high score on the Functional Independence Measure indicates functional independence.
Schoppen et al. (1999) examined the validityThe degree to which an assessment measures what it is supposed to measure.
of the TUG by comparing it to the Sickness Impact Profile-68 item scale (de Bruin, Diederiks, de Witte, Stevens, & Philipsen, 1994), and the Groningen Activity Restriction Scale (GARS) (Kempen, Doeglas, & Suurmeijer, 1993) in 32 patients over the age of 60 with unilateral transtibial or transfemoral amputation because of peripheral vascular disease. An adequate Spearman correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases - for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases - for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
was reported between the TUG and the Groningen Activity Restriction Scale (r = 0.39). The TUG also correlated adequately with the total score of the Sickness Impact Profile (r = 0.40) and mobility control and mobility range (r = 0.46 and 0.36). A poor correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases - for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases - for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
between the TUG and the subscales of the “psychic autonomy and communication” (r = 0.31), “social behavior” (r = 0.19), and “emotional stability” (r = -0.04) of the Sickness Impact Profile was found. The findings confirm that the TUG is not a reflection of mental functioning.
Noren et al. (2001) administered various assessments of balance to 65 patients with peripheral arthritis and found that the Berg Balance Scale (Berg, Wood-Dauphinee, Williams, & Maki, 1989) and the TUG had an excellent correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases - for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases - for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
(Spearman’s rho = -0.83). The correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases - for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases - for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
is negative because a high score on the Berg Balance Scale indicates normal balance, whereas a high score on the TUG indicates abnormal functioning.
Ng and Hui-Chan (2005) administered the TUG to 10 healthy elderly participants and 11 patients with chronic strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain.. Spearman correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases - for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases - for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
analyses were conducted to examine the convergent and discriminant validityMeasures that should not be related are not. Discriminant validity examines the extent to which a measure correlates with measures of attributes that are different from the attribute the measure is intended to assess.
of the TUG with various measures. No significant associations between the TUG and spasticityInvoluntary muscle tightness and stiffness that can occur after a stroke. It is characterized by exaggerated deep tendon reflexes that interfere with muscular activity, gait, movement, or speech. Spasticity can increase initially but wane down later on, after stroke.
of ankle plantarflexors of both affected and unaffected legs were observed. An excellent correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases - for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases - for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
between the TUG and the peak plantarflexion torque generated by maximum isometric voluntary contraction (MIVC) of the affected plantarflexors was reported (r = -0.86), however the TUG did not correlate with the other MIVC parameters measured. Excellent negative correlations were found between the TUG and gaitThe pattern of walking, which is often characterized by elements of progression, efficiency, stability and safety.
velocity in both healthy participants and patients with strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. (r = 0.98 and r = 0.99, respectively). For the other gaitThe pattern of walking, which is often characterized by elements of progression, efficiency, stability and safety.
parameters, the step lengths of both the affected and unaffected legs had excellent correlations with the TUG (ranged from r = -0.67 to r = -0.80). An excellent correlationThe extent to which two or more variables are associated with one another. A correlation can be positive (as one variable increases, the other also increases - for example height and weight typically represent a positive correlation) or negative (as one variable increases, the other decreases - for example as the cost of gasoline goes higher, the number of miles driven decreases. There are a wide variety of methods for measuring correlation including: intraclass correlation coefficients (ICC), the Pearson product-moment correlation coefficient, and the Spearman rank-order correlation.
was found between the distance covered during the 6-Minute Walk Test (6MWT) (Guyatt et al., 1985) and the TUG (r = -0.96). Some correlations are negative because a high score on the TUG indicates abnormal functioning whereas a high score on other measures indicate a high level of performance.
Flansbjer et al. (2005) examined 6 gaitThe pattern of walking, which is often characterized by elements of progression, efficiency, stability and safety.
performance tests in patients with mild to moderate post-stroke hemiparesis (Comfortable GaitThe pattern of walking, which is often characterized by elements of progression, efficiency, stability and safety.
Speed; Fast GaitThe pattern of walking, which is often characterized by elements of progression, efficiency, stability and safety.
Speed, Stair Climbing Ascend; Stair Climbing Descend; 6-Minute Walk Test). They found excellent correlations between the TUG and the other gaitThe pattern of walking, which is often characterized by elements of progression, efficiency, stability and safety.
performance measures examined twice, 7 days apart, ranging from r = -0.84 to r = -0.92 (these correlations are negative because a high score on the TUG indicates abnormal functioning, whereas a high score on other gaitThe pattern of walking, which is often characterized by elements of progression, efficiency, stability and safety.
measures indicate normal performance). Taken together with the results from the study by Ng and Hui-Chan (2005), the TUG appears to be a valid measure for use in patients with strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain..
Known groups:
Brooks et al. (2006) examined the construct validityReflects the ability of an instrument to measure an abstract concept, or construct. For some attributes, no gold standard exists. In the absence of a gold standard , construct validation occurs, where theories about the attribute of interest are formed, and then the extent to which the measure under investigation provides results that are consistent with these theories are assessed.
of the TUG in 52 frail older individuals. They found that the TUG could distinguish patients using different ambulatory aids. Berg et al. (1992) found that the TUG was able to distinguish between elderly individuals who walked with an aid (cane or walker) versus those who did not use any walking aid (effect sizeEffect size (ES) is a name given to a family of indices that measure the magnitude of a treatment effect. Unlike significance tests, these indices are independent of sample size. The ES is generally measured in two ways: as the standardized difference between two means, or as the correlation between the independent variable classification and the individual scores on the dependent variable. This correlation is called the "effect size correlation".
= 1.02).
Rockwood et al. (2000) examined the validityThe degree to which an assessment measures what it is supposed to measure.
of the TUG using Phase 2 data from the Canadian Study of Health and Ageing. They reported that cognitively unimpaired clients could perform the TUG faster than cognitively impaired clients (12 seconds versus 15 seconds, on average).
Morris et al. (2001) found that the TUG could distinguish between patients with Parkinson’s disease who were on the medication levodopa and those patients who were not on levodopa when compared to individuals without Parkinson’s disease.
Ng and Hui-Chan (2005) found that the TUG was able to distinguish healthy elderly individuals from patients with strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain. (mean time to complete the TUG was 9.1 seconds for healthy individuals and 22.6 seconds for patients with strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain.).
Sensitivity and Specificity:
Shumway-Cook, Brauer, and Woollacott (2000) compared the specificitySpecificity refers to the probability that a diagnostic technique will indicate a negative test result when the condition is absent (true negative).
of the TUG in predicting falls in community dwelling older adults. The TUG correctly classified 13/15 fallers (87% sensitivitySensitivity refers to the probability that a diagnostic technique will detect a particular disease or condition when it does indeed exist in a patient (National Multiple Sclerosis Society). See also "Specificity."
) and 13/15 nonfallers (87% specificitySpecificity refers to the probability that a diagnostic technique will indicate a negative test result when the condition is absent (true negative).
). These results suggest that the TUG is a sensitive and specific measure for identifying elderly individuals who are prone to falls.
Whitney, Marchetti, Schade, and Wrisley (2004) examined the sensitivitySensitivity refers to the probability that a diagnostic technique will detect a particular disease or condition when it does indeed exist in a patient (National Multiple Sclerosis Society). See also "Specificity."
and specificitySpecificity refers to the probability that a diagnostic technique will indicate a negative test result when the condition is absent (true negative).
of the TUG in 103 patient charts of those with vestibular disorders and a history of falls. SensitivitySensitivity refers to the probability that a diagnostic technique will detect a particular disease or condition when it does indeed exist in a patient (National Multiple Sclerosis Society). See also "Specificity."
(80%) and specificitySpecificity refers to the probability that a diagnostic technique will indicate a negative test result when the condition is absent (true negative).
(56%) were calculated for TUG scores of > 11.1 seconds.
Responsiveness
Brooks, Davis, and Naglie (2006) examined the responsivenessThe ability of an instrument to detect clinically important change over time.
of the TUG in 52 frail older individuals. The TUG demonstrated a large responsivenessThe ability of an instrument to detect clinically important change over time.
to an intervention that occurred between admission and discharge with a standardized response meanThe standardized response mean (SRM) is calculated by dividing the mean change by the standard deviation of the change scores.
(SRM) of 1.1.
Flansbjer et al. (2005) examined the responsivenessThe ability of an instrument to detect clinically important change over time.
of the TUG in 50 individuals with strokeAlso called a "brain attack" and happens when brain cells die because of inadequate blood flow. 20% of cases are a hemorrhage in the brain caused by a rupture or leakage from a blood vessel. 80% of cases are also know as a "schemic stroke", or the formation of a blood clot in a vessel supplying blood to the brain.. The smallest real difference (SRD), representing the smallest change that indicates a real (clinical) improvement, was small (SRD = 23%). In other words, the TUG can be used to detect clinically relevant small changes.
Salbach and colleagues (2001) examined the most responsive measure of gaitThe pattern of walking, which is often characterized by elements of progression, efficiency, stability and safety.
speed from a variety of measures in 50 post-stroke patients with gaitThe pattern of walking, which is often characterized by elements of progression, efficiency, stability and safety.
deficits. The TUG demonstrated significant change from 8 – 38 days post-stroke (SRM = 0.73). However, there were significant difficulties in obtaining scores since not all patients could complete the test at both times. The SRM reported reflects scores for only those subjects who were able to perform the test. The responsivenessThe ability of an instrument to detect clinically important change over time.
of the TUG also varied depending on the group of patients tested. In the moderate group, the TUG was rated the third most responsive tool after the 5-minute Walk Test (5mWT) (maximum pace), and the 5mWT (comfortable pace). In the fast group, the TUG was rated the second most responsive tool after the 5mWT.
References
-
Berg, K. O., Maki, B. E., Williams, J. I., Holliday, P. J., Wood-Dauphinee, S. L. (1992). Clinical and laboratory measures of postural balance in an elderly population. Archives of Physical Medicine and Rehabilitation, 73, 1073-1080.
-
Berg, K., Wood-Dauphinee, S. L., Williams, J. I., Maki, B. E. (1992). Measuring balance in the elderly: Validation of an instrument. Canadian Journal of Public Health, 83(S2), S7-11.
-
Berg, K.O., Wood-Dauphinee, S., Williams, J. L., Maki, B. (1989). Measuring balance in the elderly: Validation of an instrument. Physiotherapy Canada, 41(6), 304-311.
-
Benaim, C., Perennous, D. A., Villy, J., Rousseaux, M., Pelissier, J. Y. (1999). Vaidation of a standardized assessment of postural control in stroke patients. Stroke, 30, 1862-1868.
-
Bourbonnais, D., Bilodeau, S., Lepage, Y., Beaudoin, N., Gravel, D., Forget, R. (2002). Effect of force-feedback treatments in patients with chronic motor deficits after a stroke. American Journal of Physical Medicine and Rehabilitation, 81, 890-897.
-
Brooks, D., Davis, A., Naglie, G. (2006). Validity of 3 physical performance measures in inpatient geriatric rehabilitation. Arch Phys Med Rehabil, 87, 105-110.
-
Cattaneo, D., Regola, A., Meotti, M. (2006). Validity of six balance disorders scales in persons with multiple sclerosis. Disability & Rehabilitation. 28(12), 789-795.
-
de Bruin, A. F., Diederiks, J. P. M., de Witte de, L. P., Stevens, F. C. J., Philipsen, H. (1994). The development of short generic version of the Sickness Impact Profile. J Clin Epidemiol, 47, 407-418.
-
Fillenbaum, G. G., Smyer, M. A. (1981). The development, validity, and reliability of the OARS multidimensional functional assessment questionnaire. J Gerontol, 36, 428-434.
-
Finch, E., Brooks, D., Stratford, P. W., Mayo, N. E. (2002). Physical Rehabilitations Outcome Measures. A Guide to Enhanced Clinical Decision-Making (second ed.), Canadian Physiotherapy Association, Toronto.
-
Flansbjer, U., Holmback, A. M., Downham, D., Patten, C., Lexell, J. (2005). Reliability of gait performance tests in men and women with hemiparesis after stroke. J Rehabil Med, 37, 75-82.
-
Guyatt, G. H., Sullivan, M. J., Thompson, P. J. Fallen, E. L., Pugsley, S. O., Taylor, D. W., Berman, L. B. (1985). The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J, 132, 919-923.
-
Hayes, K., Johnson, M. (2003). Measures of Adult General Performance Tests. Arthritis & Rheumatism (Arthritis Care & Research), 49(5S), S28-S42.
-
Keith, R. A., Granger, C. V., Hamilton, B. B., Sherwin, F. S. (1987). The functional independence measure: A new tool for rehabilitation. Adv Clin Rehabil, 1, 6-18.
-
Kempen, M., Doeglas. D. M., Suurmeijer, M. (1993). Het meten van problemen met zelfredzaamheid op verzorgend en huishoudelijk gebied met de Groningen Activiteiten Restrictie Schaal (GARS): een handleiding. Groningen, The Netherlands: Noordeliik Centrum voor Gezondheidsvraagstukken, NCG.
-
Linn, B. S., Linn, M. W., Gurel, L. (1968). Cumulative Illness Rating Scale. J Am Geriatr Soc, 16, 622-626.
-
Lundin-Olsson, L., Nyberg, L., Gustafson, Y. (1998). Attention, frailty, and falls: The effect of a manual task on basic mobility. Journal of the American Geriatric Society, 46, 758-761.
-
Mathias, S., Nayak, U. S., Isaacs, B. (1986). Balance in elderly patients: The “Get-Up and Go” test. Arch Phys Med Rehabil, 67, 387-389.
-
Morris, S., Morris, M. E., Iansek, R. (2001).Reliability of measurements obtained with the Timed “Up & Go” test in people with Parkinson disease. Physical therapy, 81(2), 810-818.
-
Ng, S. S., Hui-Chan, C. W. (2005). The Timed Up & Go test: its reliability and association with lower-limb impairments and locomotor capacities in people with chronic stroke. Arch Phys Med Rehabil. 86(8), 1641-1647.
-
Nikolaus, T., Bach, M., Oster, P., Schlierf, G. (1996). Prospective value of self-report and performance-based tests of functional status for 18-month outcomes in elderly patients. Aging Clin Exp Res, 8, 271-276.
-
Norén, A. M., Bogren, U., Bolin, J., Stenstrom, C. (2001). Balance assessment in patients with peripheral arthritis: Applicability and reliability of some clinical assessments. Physiother Res Int, 6, 193-204.
-
Podsiadlo, D., Richardson, S. (1991). The Timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J Am Geriatr Soc, 39, 142-148.
-
Rockwood, K., Awalt, E., Carver, D., MacKnight, C. (2000). Feasibility and measurement properties of the functional reach and the Timed Up and Go tests in the Canadian study of health and aging. J Gerontol A Biol Med Sci, 55A, M70-73.
-
Salbach, N., Mayo, N., Higgins, J., Ahmed, S., Finch, L., Richards, C. (2001) Responsiveness and predictability of gait speed and other disability measures in acute stroke. Phys Med Rehabil, 82, 1204-1212.
-
Schoppen, T., Boonstra, A., Groothoff, J. W., de Vries, J., Goeken, L. N., Eisma, W. H. (1999). The Timed “Up and Go” test: reliability and validity in persons with unilateral lower limb amputation. Arch Phys Med Rehabil, 80, 825-828.
-
Schoppen,T., Boonstra, A., Groothoff, J. W., de Vries, J., Goeken, L. N., Eisma, W. H. (2003). Physical, mental, and social predictors of functional outcome in unilateral lower-limb amputees. Archives of Physical and Medical Rehabilitation, 84, 803-811.
-
Schwartz, A. V.,Villa, M. L.,Prill, M., Kelsey, J. A., Galinus, J. A., Delay, R. R., Nevitt, M. C., Bloch, D. A., Marcus, R., Kelsey, J. L. (1999). Falls in older Mexican-American women. J Am Geriatr Soc, 47, 1371-1378.
-
Siggeirsdottir, K., Jonsson, B. Y., Jonsson, H., Iwarsson, S. (2002). The “Timed Up & Go” is dependent on chair type. Clinical Rehabilitation, 16(6), 609-616.
-
Shumway-Cook, A., Brauer, S., Woollacott, M. (2000). Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther, 80, 896-903.
-
Shumway-Cook, A., Woollacott, M. H. (2001). Motor Control: Theory and Practical Applications (second Ed). Lippincott Williams & Wilkins. pp272-273.
-
Steffen, T. M., Hacker, T. A., Mollinger, L. (2002). Age-and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys Ther, 82(2), 128-137.
-
Thompson, M., Medley, A. (1995). Performance of Community Dwelling Elderly on the Timed Up and Go test. Physical and occupational therapy in geriatrics, 13, 17-30.
-
Tinetti, M. E. (1986). Performance-oriented assessment of mobility problems in elderly patients, J Am Geriatr Soc, 34, 119-126.
-
Tremblay, L. E., Savard, J., Casimiro, L., Tremblay, M. (2004). Repertoire des Outils d’Evaluation en Francais pour la Readaptation, Regroupement des intervenantes et intervenants francophones en sante et enservices sociaux de l’Ontario, Ottawa.
-
Whitney, S. L., Marchetti, G. F., Schade, A., Wrisley, D. M. (2004). The sensitivity and specificity of the Timed “Up & Go” and the dynamic gait index for self-reported falls in persons with vestibular disorders. Journal of Vestibular Research, 14(5), 397-409.
See the measure
How to obtain the TUG
The TUG can be obtained by contacting the developer, Diane Podsiadlo, CLSCNDG, 2525 Boulevard Cavendish, Bureau 110, Montreal, QC, H4B 2Y4. Fax: 514-485-6406.
By clicking here, you can access a video showing how to administer the assessment.